Article of the week: Smaller is better? Microperc comes of age
Micropercutaneous nephrolithotomy (microperc) vs retrograde intrarenal surgery for the management of small renal calculi: a randomized controlled trial
Ravindra B. Sabnis, Raguram Ganesamoni, Amit Doshi, Arvind P. Ganpule, Jitendra Jagtap and Mahesh R. Desai
Department of Urology, Muljibhai Patel Urological Hospital, Nadiad, Gujarat, India
OBJECTIVE
• To compare micropercutaneous nephrolithotomy (microperc) and retrograde intrarenal surgery (RIRS) for the management of renal calculi <1.5 cm with regard to stone clearance rates and surgical characteristics, complications and postoperative recovery.
PATIENTS AND METHODS
• Seventy patients presenting with renal calculi <1.5 cm were equally randomized to a microperc or a RIRS group between February 2011 and August 2012 in this randomized controlled trial. Randomization was based on centralized computer-generated numbers. Patients and authors assessing the outcomes were not blinded to the procedure.
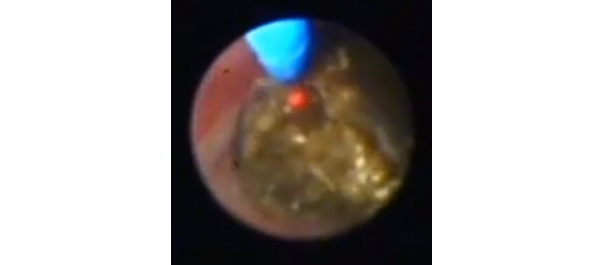
• Microperc was performed using a 4.85-F (16-gauge) needle with a 272-μm laser fibre. RIRS was performed using a uretero-renoscope.
• Variables studied were stone clearance rates, operating time, need for JJ stenting, intra-operative and postoperative complications (according to the Clavien–Dindo classification system), surgeon discomfort score, postoperative pain score, analgesic requirement and hospital stay.
• Stone clearance was assessed using ultrasonography and X-ray plain abdominal film of kidney, ureter and bladder at 3 months.
RESULTS
• There were 35 patients in each group. All the patients were included in the final analysis.
• The stone clearance rates in the microperc and RIRS groups were similar (97.1 vs 94.1%, P = 1.0).
• The mean [sd] operating time was similar between the groups (51.6 [18.5] vs 47.1 [17.5], P = 0.295). JJ stenting was required in a lower proportion of patients in the microperc group (20 vs 62.8%, P < 0.001). Intra-operative complications were a minor pelvic perforation in one patient and transient haematuria in two patients, all in the microperc group. One patient in each group required conversion to miniperc.
• One patient in the microperc group needed RIRS for small residual calculi 1 day after surgery. The decrease in haemoglobin was greater in the microperc group (0.96 vs 0.56 g/dL, P < 0.001). The incidence of postoperative fever (Clavien I) was similar in the two groups (8.6 vs 11.4%, P = 1.0). None of the patients in the study required blood transfusion.
Read Previous Articles of the Week