Posts
Residents’ podcast: MIMIC Study
Part of the BURST/BJUI Podcast Series
Mr Chuanyu Gao is a Core Surgical Trainee in KSS Deanery. He graduated from UCL Medical School and obtained his iBSc in Surgical Sciences before completing his Academic Foundation Years in East of England Foundation School. Chuanyu first became involved with BURST on the MIMIC Study as an international site coordinator and has been part of the BURST committee ever since.
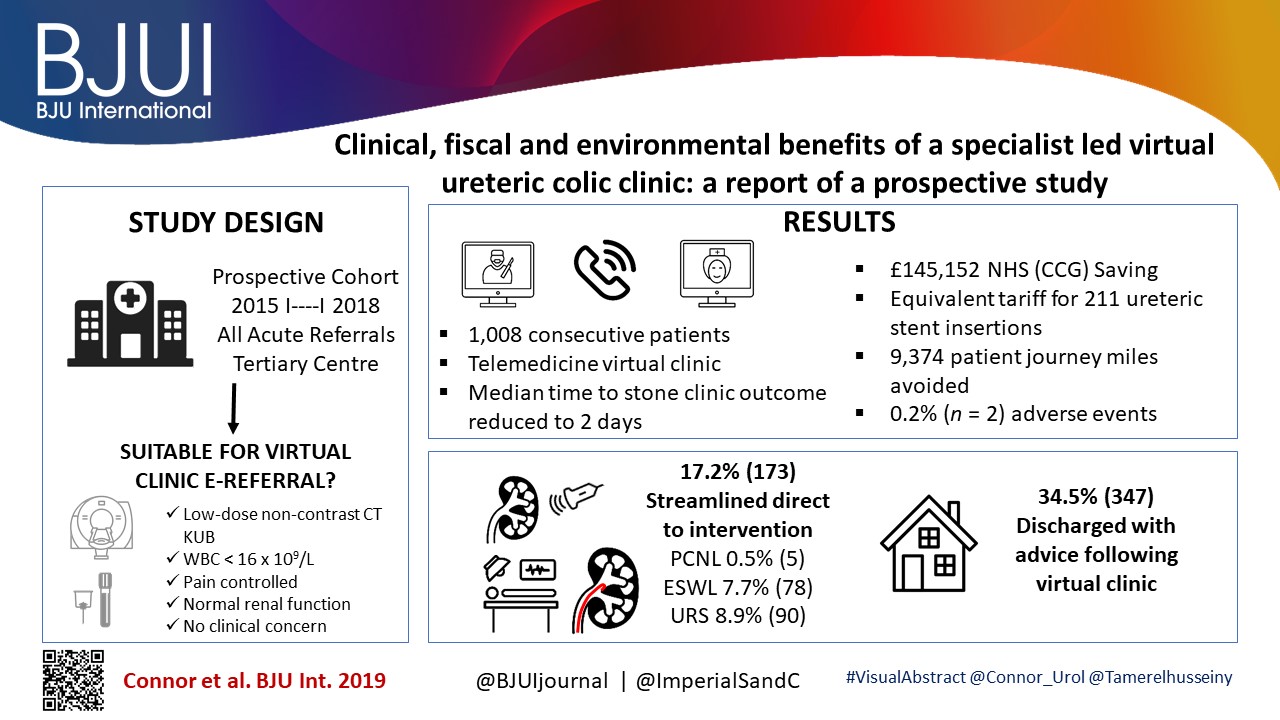
Factors associated with spontaneous stone passage in a contemporary cohort of patients presenting with acute ureteric colic: results from the Multi‐centre cohort study evaluating the role of Inflammatory Markers In patients presenting with acute ureteric Colic (MIMIC) study
SIU Congress Highlights – Lisbon 2017
Olá! The 37th Congress of the Société d’Urologie (SIU) was held in Lisbon, a beautiful, historic city (19th-22nd October 2017). It is the first time the congress has been held here. We were told by the co-hosts during the opening ceremony that Portugal has a history of finding new routes and building bridges to other cultures, which they hoped to emulate at the Congress. The iconic 24 de Abril Bridge, the largest in Europe, was visible from the Congress Centre serving as a visual reminder of bridges being made during this congress.
The SIU is unique as it is a truly international association with no country or continent affiliation; it has 7000 members from 130 countries and 24 directors from every continent. Therefore the congress brings urologists from all over the world together. The words “Together, United, Stronger” said during the opening ceremony resonated as the ethos of the conference; and is especially pertinent in the current worldwide political climate. Furthermore, that the educational, global and philanthropic aspects of being part of such a society was highlighted as ways we can all help each other.
SIU 2017 had an engaging scientific programme providing a valuable educational experience to attendees over the four days. It covered the breadth of urology and we were honoured to listen to such notable speakers. The navigable congress centre (as well as the congress being a smaller meeting, as compared to EAU, AUA) meant delegates could easily attend whatever took their interest. The Scientific Programme included Plenary sessions, Master Classes, debates, ‘controversies’ sessions, instructional courses, poster presentations, the SIU Nurses’ Symposium and hosted urological organisation meetings. There were also Industry supported sessions and an Exhibition Hall.
The social programme allowed relaxation and networking amongst colleagues; plus sampling local Portuguese wines, food and an insight into Portuguese culture. The opening ceremony included a Fado performance. The SIU night held at Pátio da Galé in the PraÇa do Comércio was the pinnacle of the social aspect of the conference. The refreshments were plentiful and delicious, there were gelato stands as well as enough Pastel de Nata to feed a small army! A typical brass band, ceramic station, football net and DJ kept people entertained until we were told to leave. The SIU President’s Dinner held in the Queluz Palace was an amazing night in impressive surroundings for invited guests.
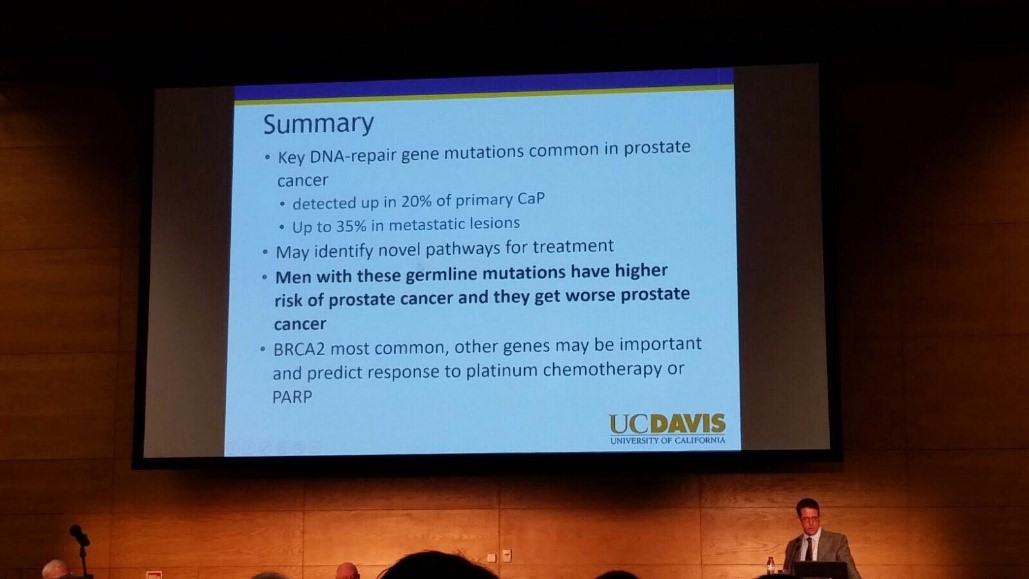
The fully attended WUOF session on the first day brought experts in the field of Urological cancers to provide their views on the changing paradigms and new treatments. All talks provided succinct, expert opinion. The presentation by Marc Dall’Era on the genetics of prostate cancer and link with the BRACA gene was particularly informative; especially as these men get worse cancer: pictured. Genetic counselling of patients diagnosed with prostate cancer may need to increase in the future. Genomics was discussed in other cancer sessions too; it’s growing availability, reducing costs and correlation with difference in outcomes between patients must surely strengthen the argument for more personalised medicine.
I also particularly enjoyed the presentation by Tony Finelli who unraveled the notion of ‘surgical outcome’ which is often used to analyse the quality of surgery; this is then used in arguments for high volume centres. He suggested instead that assessing quality needs Quality Indicators and one alone isn’t sufficient. His group in Canada used their national database to propose 32 Quality Indicators, which are valid, reliable, feasible and useable; they found that higher quality had lower mortality and morbidity. Patient centred care, patient selection, high quality surgery and recovery was a common theme in other sessions too.
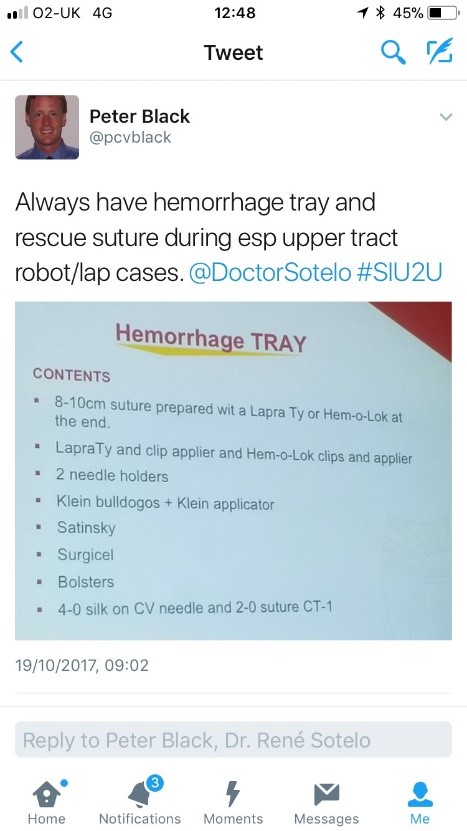
The SIU Innovators Symposium didn’t disappoint; highlights included Dr Sotelo’s presentation of ‘sticky situations’ in robotic surgery. His operative videos showed all the things you really don’t want to see whilst operating, however he and the panel provided tips in order to avoid or correct these operative mistakes. Dr Sotelo’s advice regarding having a ‘haemorrhage tray’ present was ingenious and useful: pictured. Thank you to Dr Sotelo and Dr Knudsen who shared their operative videos with us in order to provide this learning; mistakes in surgery should be shared to avoid others making the same mistakes. The symposium also invited two influential leaders, Professor Prokar Dasgupta, editor BJUI, and Professor Arnulf Stenzl to give their approach on leadership. Prof Stenzl suggested it was easier to explain how not to be a bad leader as he has learnt more from his mistakes than from successes. Prof Dasgupta suggested his leadership style was to be collaborative, trusting team members to deliver, democratic and transformative; also that he, as a leader, wanted to “help other people do well”.
SIU had a strong presence of trainees; many attending to present their academic work during the moderated poster sessions, listen to worldwide experts and of course network with others from around the world and generating future collaborations. One session ‘Sage Advice from the Wise’ was particularly aimed at trainees’ where Urological trainees met 10 experts (all wise, but certainly not old!). We were able to discuss career plans, ask questions about fellowships and talk about the advantages of academia alongside clinical practice. There was also a Residents Rapid Fire Q&A which was won by Dr Avinash Odugoudar: pictured.
Urological cancer treatment featured heavily on the programme. One particularly inspiring talk on advanced testicular cancer by one of the leading surgeons in Europe, Axel Heidenreich, really expanded our horizons of just what can be achieved operatively for patients with metastatic disease, including aortic resection and Whipple’s procedure. It proves that big, open surgery does exist in urology for the right patients; requiring expertise and courageous surgical skills but offering patients treatment despite disseminated disease. One session included debating the use of routine radiation for positive surgical margins in prostate cancer. The presentations by Dr Dall’Ezra and Dr Briganti actually came to very similar conclusions. Both wanted to avoid over treatment and championed a risk stratified approach with emphasis on patient selection; as not all those with positive margins recur. It was suggested that choosing those at greatest risk of recurrence for example the site(s) of positive margin, high Gleason score, early rise in PSA (even if remains less than 0.5) and ultra-sensitive PSA can help to stratify need for adjuvant radiotherapy; or alternatively monitor with option for salvage treatment.
Robotic assisted surgery for prostatectomy, cystectomy and nephrectomy was debated freely throughout the congress. Most quoted recent evidence that there is no clear advantage with regards to blood loss, LOS, long term outcomes and survival; but very different costs. Dr Mihir Desai argued that if you already had the robot you should encourage high volume surgery, but that departments have a responsibility to put the robot to good use; not for simple cases, but rather be reserved for difficult operations so the real advantages of robotic assisted surgery will be better appreciated. Criticism was made of RCTs not being the right research method for comparing surgical techniques as it leads to comparison of individuals not techniques. We eagerly anticipate the iROC study. An important point made regarding robotic cystectomy was that it must include intra-corporeal bladder formation, otherwise many of the advantages of the minimally invasive part are lost. Laparoscopic surgery was argued as not old fashioned; but rather an efficient and cost effective method of minimal access surgery without compromising on outcomes. However open surgery is still an option in many hospitals worldwide; a question from the audience included the dilemma faced by departments whose similar outcomes between open and laparoscopic procedures do not justify the switch to laparoscopy.
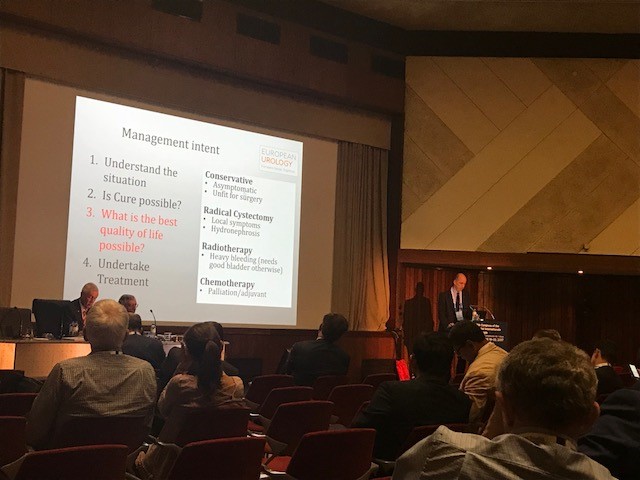
Prof Catto, editor of European Journal of urology delivered a compelling presentation of the advantages of radical cystectomy over radiotherapy for locally advanced bladder cancer. He also mentioned the importance of surgical planning and management intent: pictured. In some cases he does pre-operative MRI, however a PET scan when organised, doesn’t necessarily change his management. He also presented a plenary lecture on risk factors for upper tract TCC which confirmed smoking as the number one risk as well as occupation. However combustion occupations and amine-relate occupations show a difference in cancer aggression suggesting the biology of the cancer is different. Like others, he wanted to aim for personalised treatment of cancer with specific treatments according to genotype.
Debating the merits of surgery was a common theme in several sessions, perhaps unsurprisingly. However a particular highlight was the debate of medical vs surgical theory for lichen sclerosis (LS). The clear and compelling argument by Bradley Erickson for medical treatment rested on 10 points, which included: that LS is an inflammatory condition and these are not necessarily managed by surgery, the dermatologist and gynaecologist manage LS without surgery, LS in the urethra demonstrates squamous change which is reversible and lastly that we don’t really fully understand this disease yet.
Female urology was the first plenary session of the congress and the use of mesh unsurprisingly featured in other sessions, included one entitled ‘controversies in urology’. The clear message from Dr Badlani was to know the anatomy and not to ‘have a go’ at continence surgery, it needs expertise. He and his panel presented difficult cases including mesh seen at cystoscopy, operative video of hydro-dissection and an image of compete extrusion which led the audience to wonder if it had even been placed correctly in the first place!?
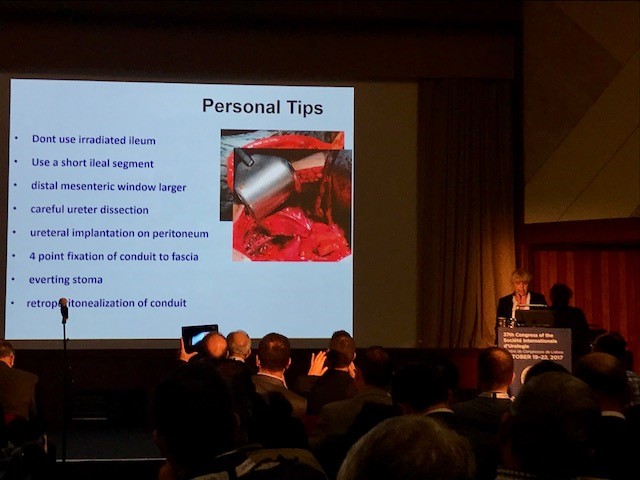
In the joint SIU-GURS meeting panel members each presented a challenging case from their experience of reconstructive surgery and ileal conduit formation; then this was discussed amongst the panel. There was an amazing X-ray of a huge stone in an ileal conduit due to stasis of urine, confirming the need to avoid long conduits. A fear held by many was early failure of the anastomosis; when debating when to re-operate, I particularly liked the phrase “three months to let the belly cool down” said with an American drawl. Margit Fisch shared her top tips of surgery: pictured. An insight into managing continence in patients with Spina Bifida was succinctly presented by Sean P. Elliot; he advised that the patients needed to be ‘proud of their stoma’ and that each needed an individual surgical plan but holistic approach.
Endourology and stone sessions were well attended and each explored different treatment modalities for stone management. Plus the congress offered masterclasses for ureteroscopic techniques, the joint SIU-Endourology session, poster sessions and a ‘controversies session’ debating URS vs Mini-perc. There was also an instructional course on lasers and flexible ureteroscopic technique. Experienced surgeons from across the globe argued for and against the role of ESWL vs RIRS vs PCNL in modern practice. Aside from patient and stone factors there was an appreciable point made of the importance of surgeon experience and available resources of the institution. Non-surgical aspects of stones were also presented, such as diet and hydration in stone disease. Advances in stone surgery, including a robotic assisted ureteroscope was particular enlightening and futuristic; however brought up the inevitable dilemma of clinical need for such technology at a time of financial restraint facing many healthcare systems.
Andrology sessions included a joint SIU-ISSM session, a master class on urethral stricture disease, video session on male reconstruction and poster session on sexual function and dysfunction. There was a debate on the role of the urologist in the management of male infertility and improving sperm. The (interesting) use of an acronym F.A.S.T was described by host urologist from Portugal Dr Pedro Vendeira: pictured. This is in relation to the follow up of non-responders to PDE-5 inhibitors, of which non responders were those who had tried these medications more than eight times. He described a 50% drop out of the use of these drugs due to cost, side effects and co-morbidities. The difficulty of treating Peyronies was discussed by Dr Moncada who confirmed the absence of the role for medical therapies, except use of PDE-5 inhibitors to strengthen erections. There was a role for ‘ penile rehabilitation’ which included a (peculiar) traction device. He presented his and the EAU indications for surgery and he stressed the importance of managing patient expectation and informed consent.
In conclusion, the SIU Congress was both informative and enjoyable. Our co-hosts promises: of warmth, friendship and the Portuguese tradition of sharing wine were delivered alongside a beneficial education programme. Those that did not attend can access abstracts and lectures online via the SIU@U platform.
SIU are also increasing their activities with the following initiatives: ‘B2B’ bench to bedside, ‘Uro-Technology’ training and ‘U-care’ a global urological research collaboration. SIU also wants to build on the opportunities for global education and global health; plus help colleagues without same level of resources.
Thank you to the SIU organisers for a successful congress! Thank you to the presenters and speakers for their expertise and dedication to academia in urology; and congratulations to all the prize winners. I’m sure the next SIU Congress 2018 in South Korea will be equally successful.
Adeus!
Até à próxima!
Sophie Rintoul-Hoad
Royal Society of Medicine: Key issues in Endourology
The RSM section of Urology #RSMUrology hosted a day on the Key issues in Endourology on 20th October. This was the first meeting of the academic year under President Roland Morley. Sri Sriprisad put together a complete endourology day with key subject areas of “PCNL and stones”, “upper tract TCC” and “BPH and retention”. Speakers from India, America and Spain provided expert opinions from around the globe.
The day started with the evolution of stone and urological laparoscopic surgery. Showing an insight into the challenges with the initial introduction of laparoscopic urological surgery. In order to allow surgeons the chance to discuss their experiences and troubleshoot and develop surgical techniques the SLUG forum (southern laparoscopic urology group) was created, which is still running today in the annual AUA meeting.
PCNL techniques were the subject for several debate lectures. Access for PCNL tracts was debated by Dr Janak Desai, visiting from Samved Urology hospital in India, arguing for fluoroscopic puncture with over 10,000 cases to date! Jonathan Glass, from Guy’s and St. Thomas’ Hospital, spoke for the prone position for the majority of PCNL, but selecting the supine position in 5-10% of cases depending on the anatomy and stone position. Dr Desai also spoke on ultra-mini PCNL, which he advocates using to treat solitary kidney stones under 2 cm in preference to flexible ureteroscopy.
The future of ESWL was debated and the audience voted that it is still “alive and clicking” by a narrow margin. However, although up to 80% clearance rates are quoted for upper pole stones less than 2 cm, the problem is that results of treatment are varied and unpredictable, and real-life success rates are far inferior. The variation in results may in part be due to the fact that there are no formal training courses for specialist radiographers nor SAC requirements for specialist registrars. Professor Sam McClinton presented on clinical research in stone disease with results from the TISU trial on primary ESWL vs. ureteroscopy for ureteric stones due out next year. The results will be fascinating and may help to decide if ESWL has a future in the UK.
Professor Margaret Pearle, visiting from the University of Texas Southwestern Medical Centre, explained the importance of treating residual fragments. With data showing that 20 – 36% of >2 mm residual stones after ureteroscopy required repeat surgery within 1 year. In a thought provoking lecture, she presented data showing that ureteroscopy may not be as good as we think and when critically examined, true stone-free rates maybe no better than ESWL. Maybe miniaturised PCNL is the way forward after all?
The follow up of small kidney stones is an uncertain area with very little written in either the EAU or AUA guidelines. Data from a meta-analysis by Ghani et al. shows that for every year of follow up on small kidney stones 7% may pass, 14% grow and 7% will require intervention. However, it is not possible in most health systems to follow everyone up forever and Mr Bultitude advocated increasing discharge rates from stone clinics to primary care after an agreed time of stability, allowing more on the complex and metabolic stone formers.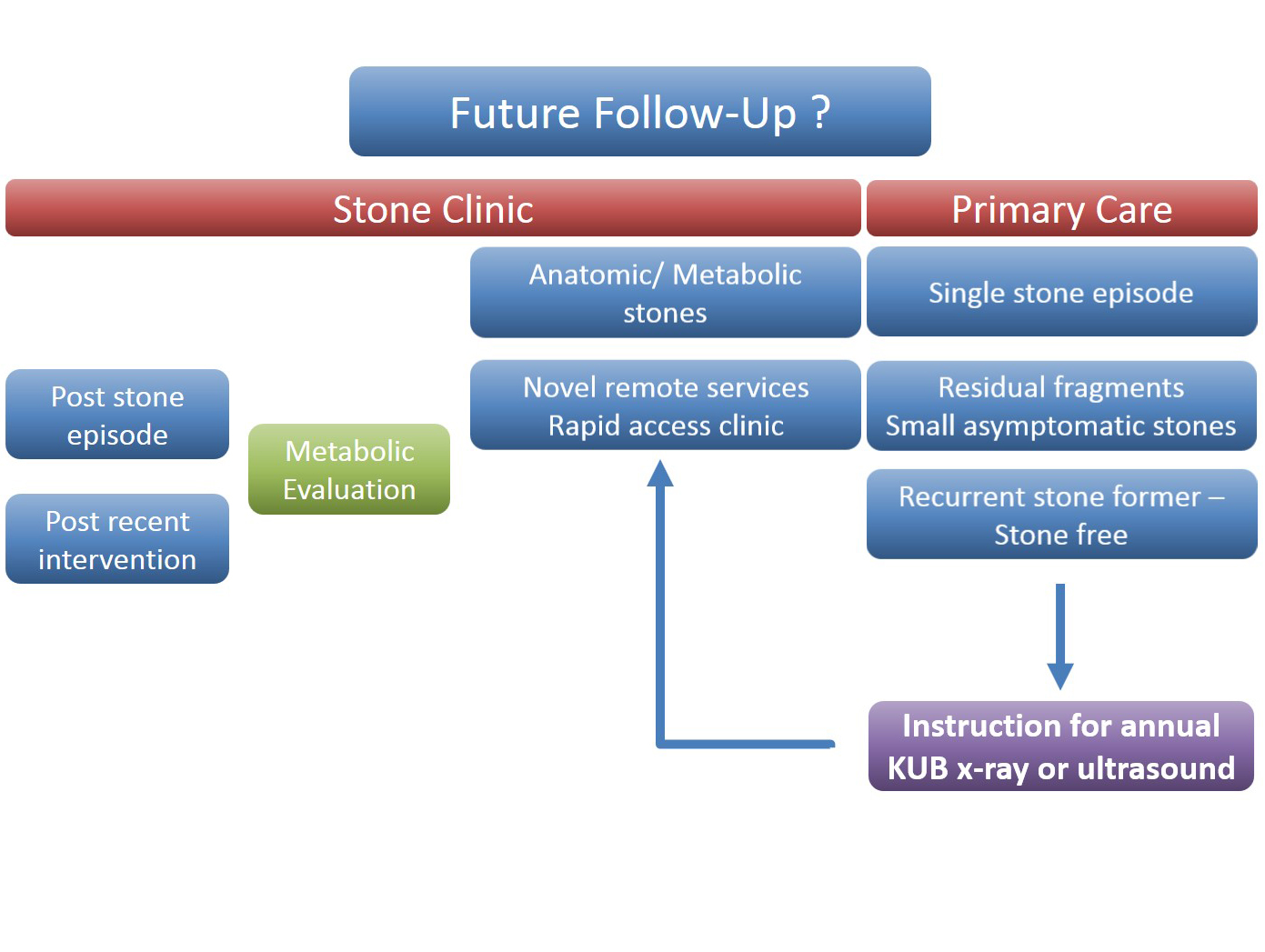 Figure 1- Stone follow up algorithm
Figure 1- Stone follow up algorithm
The expert stone panel then debated several challenging cases including “the encrusted stent”, stones in a pelvic kidney or calyceal diverticulum. These cases certainly are a challenge and require an individualized approach usually with multi-modality treatments.
Figure 2 – Stone expert panel
Upper tract urological biopsies are notoriously inaccurate, with only 15% of standard biopsies quantifiable histologically. Low grade tumours, are potentially suitable for endoscopic management with laser ablation. Dr Alberto Breda, from the urology department of Fundacio Puigvert Hospital in Spain, presented a novel solution for the future. This promising new technology uses confocal endomicroscopy to grade upper tract urological cancer. Initial results show 90% accuracy in diagnosing low grade tumours, which could then be safely managed endoscopically avoiding nephron-ureterectomy for some patients.
Figure 3 – Confocal endomicroscopy for upper tract malignancy
In the final session, a debate on BPH treatment, the audience preferred the bipolar resection technique for treating “the 60 year old with retention, with a 90 gram prostate and on rivaroxaban”, although HOLEP came a close second, with that talk giving the quote of the day “I spend more time with the morcellator than the wife.”
Figure 4 – Bipolar TURP wins the day
Nishant Bedi
ST4 Specialist urology registrar
Highlights from the Urological Association of Asia Annual Congress 2017
Having trained and worked in London throughout my urology career, I have recently relocated and joined the exciting, dynamic urology community of my birthplace, Hong Kong. Coincidentally, it so happens to be this year’s host of the Urological Association of Asia (UAA) annual congress #UAA2017.
The beautiful and mesmerising night view of the Victoria Harbour of Hong Kong.
Established in 1990 in Fukuoka, Japan, the #UAA currently has 25 urological associations as members or affiliated members across Asia and Australasia with and over 25,000 members. This was my attendance at the #UAA and it most certainly did not disappoint. What made the conference even more special was the chance to meet up with my good friend and ex-colleague from Guy’s Hospital @nairajesh – both of us were honoured to speak at the meeting. With over 1600 delegates attending the meeting and over 500 scientific abstracts presented, the congress served as an excellent platform for knowledge exchange and the establishment of professional links with many urological greats in Asia and beyond.
Pre #UAA2017 Congress Activities
#UAA2017 started off with a pre-congress ‘wet-lab’ 3D laparoscopic skills and endourology workshop hosted by @HKUniversity and the European School of Urology @UrowebESU. Both transperitoneal laparoscopic and retroperitoneoscopic techniques were taught by eminent leaders and pioneers in minimally invasive urological surgery by faculties from Europe, India and China, including Professor Jens Rassweiller, Professor Christian Schwentner (@Schwenti1977), Dr Domenico Veneziano (@d_veneziano), Professor Janak Desai (@drjanajddesai), and Professor Zhang Shudong.
Joint UAA-ESU 3D laparoscopic and endourological skills course faculties. Left to right: Dr Ada Ng (Hong Kong), Dr Wayne Lam @WayneLam_Urol (Hong Kong), Professor Janek Desai @drjanajddesai (India), Professor Jens Rassweiller (Germany), Professor MK Yiu (Hong Kong), Dr James Tsu (Hong Kong), Dr WK Ma (Hong Kong).
Joint UAA-ESU 3D Laparoscopic skills workshop – Above: Professor Rassweiller (Germany) supervising overseas delegates. Below: Professor MK Yiu (Hong Kong) demonstrating techniques of laparoscopic suturing to delegates from China.
The renal cell carcinoma #RCC masterclass was a particular highlight. A whole day of excellent lectures and speakers entertained both local and international delegates, and was particularly popular with trainees. There were talks examining the role of percutaneous biopsy of renal tumours presented by Alessandro Volpe (@foxal72), an update of current trends and techniques in robotic and laparoscopic partial nephrectomy by Dr. Joseph Wong (Hong Kong) and Dr. Shuo Wang (China) and a fantastic discussion examining the role of non-clamping partial nephrectomy by Dr. Ringo Chu (Hong Kong). The afternoon session kicked off with @nairajesh giving a comprehensive review on the surgical management of advanced #RCC. Professor Axel Bex (Netherlands) continued with an examination of neoadjuvant and adjuvant systemic therapy in #RCC and the emerging role of #immunotherapy. Professor Alessandro Volpe (@foxal72) discussed the current #EAU guidelines and recent updates.
Masterclass in #RCC: @foxal72 , @nairajesh , Professor Axel Bex (Netherlands), with moderators Dr Ringo Chu (Hong Kong) and Dr Joseph Wong (Hong Kong).
Day 1 of #UAA2017
The plenary session on day 1 of #UAA started off with Professor Zengnan Mo from China on the epidemiology of prostate cancer in Asia. There is, not surprisingly, a very diverse range of incidence of #prostatecancer rate across the largest continent in the world, inevitably effected by the presence of #PSA screening in countries such as Japan and Korea, ethnicity (East Asia vs Middle East), genetics (Israeli Jewish population), and their local healthcare system and policies. Arguably the currently available #prostatecancer screening trials may not be applicable to the Asian populations, and various on-going studies in Japan and China are going to address these issues. One in particular is an ongoing population-based study funded by the Chinese Ministry of Science and Technology, in which over 50,000 men will be recruited into the screening, early detection, localised, and advanced #prostatecancer cohorts and to be followed up with time. Obviously, we will not expect to see the results of the trial anytime soon, but will surely answers to address the behaviour of prostate cancer in the Asian population in the future.
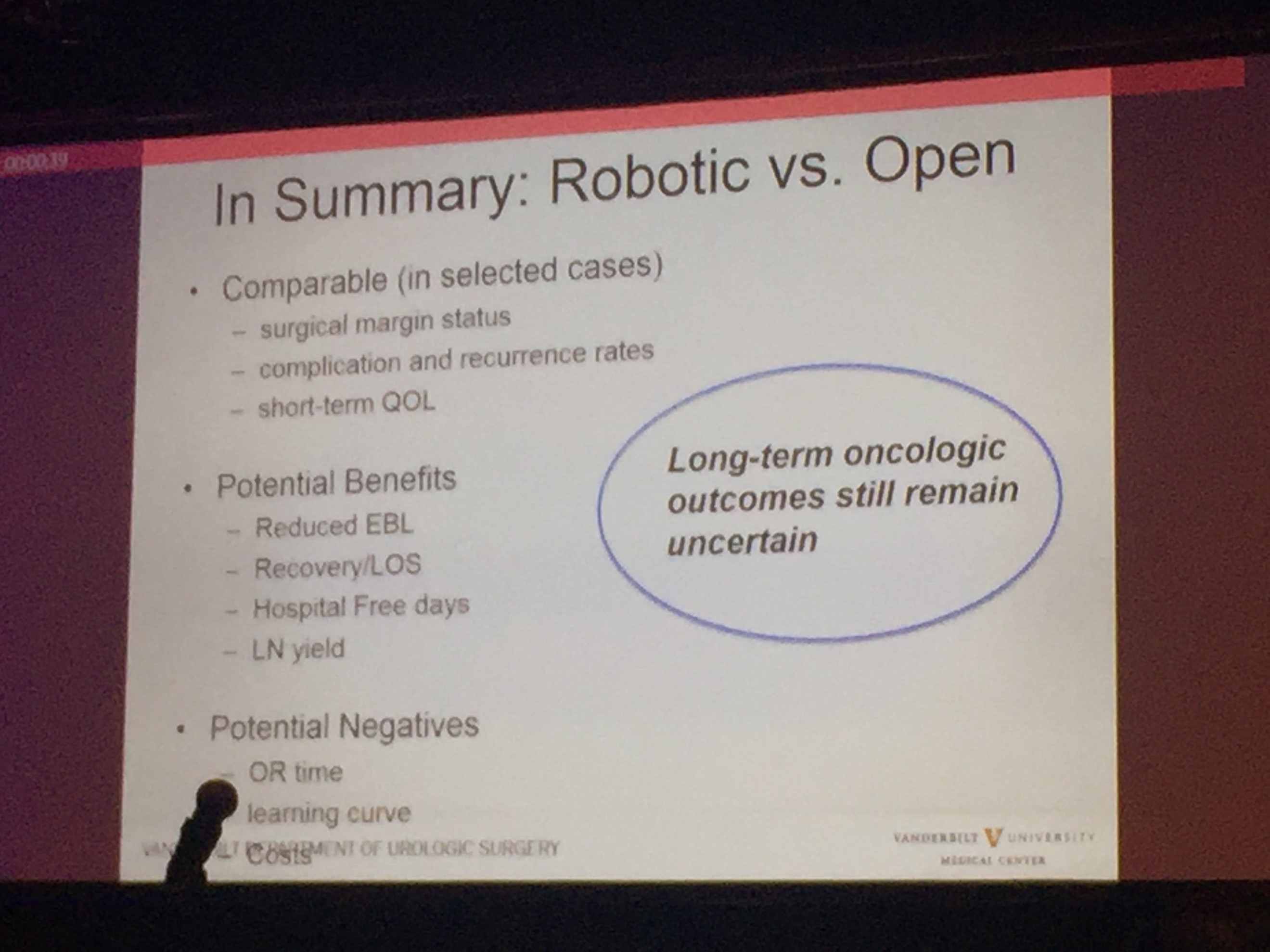
Professor Sam Cheng (@UroCancerMD) from Vanderbilt University then gave a comprehensive review on the current status of #cystectomy. Robotic cystectomy appears to have the benefit of reduced blood loss and length of stay. However, long-term oncological outcome still remains uncertain, and certainly, patient reported outcome measures (PROMs) is lacking.
Day 2 of #UAA2017
After early showers on day 2 of UAA, Hong Kong was heating up with temperatures over 33 degrees Celsius. So were the discussions in the plenary session in the morning. Professor Freddie Hamdy (@Freddie_Hamdy) gave the #EAU lecture on #activesurveillance for #prostatecancer. This was followed on nicely with the current status of #prostatecancer management in Hong Kong by Dr. Yau-Tung Chan and Dr. Gerhardt Attard (UK) enlightened the audience with a concise update in the management of hormone sensitive prostate cancer, an area where the landscape is ever-changing.
The advanced oncology session started off with a heated debate in the use of mass clamping (Dr Ringo Chu, Hong Kong) versus selective artery clamping in partial nephrectomy (Dr Tae-Gyun Kwon, Korea). Both speakers presented with very valid arguments and perhaps it was fair to say it ended up with all square. Professor Krishna Sethia (UK) gave a fascinating summary of the current local management of #penilecancer at centralised penile cancer centres in the UK, after which I was honoured to provide an update on current nodal management in #penilecancer from my recent experience at St George’s University Hospitals @StGeorgesTrust in the UK. It was exciting to see the centralisation of services in #penilecancer in the UK has given great opportunities to understand and optimise management of patients with such rare disease.
The Semi-live sessions entertained the audience on both days of the conference. Excellent videos were presented throughout. Professor Koon Rha of Yonsei University in South Korea gave a fantastic semi-live talk on his tricks and techniques of Retzius-space sparing Robot-assisted radical prostatectomy. Perhaps what’s even more exciting to know is that a Korean company has produced a new robot for surgery which has been well tested by Professor Rha’s group, which has just literally been licenced and approved in Korea just days before #UAA2017. Will this finally drive the cost of robotic surgery down? Time will tell.
Associate Professor Declan Murphy (@declanmurphy) and Mr. Rajesh Nair (@nairajesh) both contributed with a beautiful video showcasing techniques in total pelvic exenteration and long-term outcomes of urinary diversion and reconstruction in this cohort of patients.
The Gala dinner in the evening was full of fun and entertainment. Following the performance of a soprano quartet formed by local Hong Kong urologists (who sang the classic My Way with a twist on prostate examination!), the rock stars of urology – Professor Jens Rassweiller, Dr Samuel Yee from Hong Kong, and Dr Domenico Veneziano (@d_veneziano) provided an energetic and electrifying live performance of some rock classics!
Urology Rock N’ Roll! Left to right: Professor Jens Rassweiller (Germany), Dr Domenico Veneziano (Italy), Dr Samuel Yee (Hong Kong).
However, perhaps the highlight and the most touching moment of the evening the performance of a song written and sung by a young local former patient with a history of #ketaminebladder , who was successfully treated by the urology team lead by Professor Anthony Ng at the Prince of Wales Hospital in Hong Kong. His surgery and treatment has transformed his life – he is now enjoying a career as both a singer-songwriter of a rock band and as a footballer!
Day 3 of #UAA2017
The morning plenary session also saw the evergreen Dr Peggy Chu of Hong Kong, renown for her discovery of ketamine-associated uropathy and pioneered the management of this challenging 21st century urological disease.
Left to right: Dr CW Man (Hong Kong), Congress President of #UAA2017, and Dr Peggy Chu (Hong Kong).
She delivered a very interesting talk on revisiting the role of #gastrocystoplasty. Interestingly, the operation was first described and carried out in human by the honourable Professor CH Leong at my current institution, Queen Mary Hospital @HKUniversity , in the 1970s following a successful animal study at the same institution. Its use has been limited due to its associated metabolic disturbances, but arguably it is still a weapon that can be used when tackling patients with tuberculosis-associated severely contracted bladder, in particular those who have already been rendered to have a single solitary kidney due to the disease. Another situation when #gastrocystoplasty can still be considered are those patients with #ketamine uropathy. Although patients are usually required to be completely abstinence from #ketamine abuse for a certain lengthy period of time before they are eligible for surgical treatment, many fear the avalanche effect of ileal re-absorption of the drug if an ileo-cystoplasty has been carried out in these patients, if they happen to resume ketamine use in the future. Hence, #gastrocystoplasty may be a better substitution tissue for cystoplasty in the management of such patients.
The meeting also provided an opportunity to catch up with fellow Guy’s Hospital urology graduates @nairajesh and @declanmurphy over a cold pint of Hong Kong locally made #MoonzenBeer, when the temperature outside the conference centre was hitting 34 degrees Celsius!
Left to right: Dr Wayne Lam (Hong Kong), Mr Rajesh Nair (Australia/United Kingdom), A/Prof Declan Murphy (Australia).
All credits to #UAA and the local organisers’ immense effort and hard work, making this congress a valuable learning experience for everyone who participated. We very much look forward to #UAA2018. Bring on Kyoto, Japan!
Wayne Lam
Assistant Professor in Urology, Queen Mary Hospital, University of Hong Kong
Twitter: @WayneLam_Urol
Rajesh Nair
Fellow in Robotic Surgery and Uro-Oncology
RSM Urology Winter Meeting 2017, Northstar, California
 This year’s Annual RSM Urology Section Winter Meeting, hosted by Roger Kirby and Matt Bultitude, was held in Lake Tahoe, California.
This year’s Annual RSM Urology Section Winter Meeting, hosted by Roger Kirby and Matt Bultitude, was held in Lake Tahoe, California.
A pre-conference trip to sunny Los Angeles provided a warm-up to the meeting for a group of delegates who flew out early to visit Professor Indy Gill at the Keck School of Medicine. We were treated to a diverse range of live open, endourological and robotic surgery; highlights included a salvage RARP with extended lymph node dissection and a robotic simple prostatectomy which was presented as an alternative option for units with a robot but no/limited HoLEP expertise.
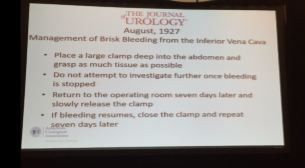
On arrival to Northstar, Dr Stacy Loeb (NYU) officially opened the meeting by reviewing the social media urology highlights from 2016. Next up was Professor Joseph Smith (Nashville) who gave us a fascinating insight into the last 100 years of urology as seen through the Journal of Urology. Much like today, prostate cancer and BPH were areas of significant interest although, in contrast, early papers focused heavily on venereal disease, TB and the development of cystoscopy. Perhaps most interesting was a slightly hair-raising description of the management of IVC bleeding from 1927; the operating surgeon was advised to clamp as much tissue as possible, close and then return to theatre a week later in the hopes the bleeding had ceased!
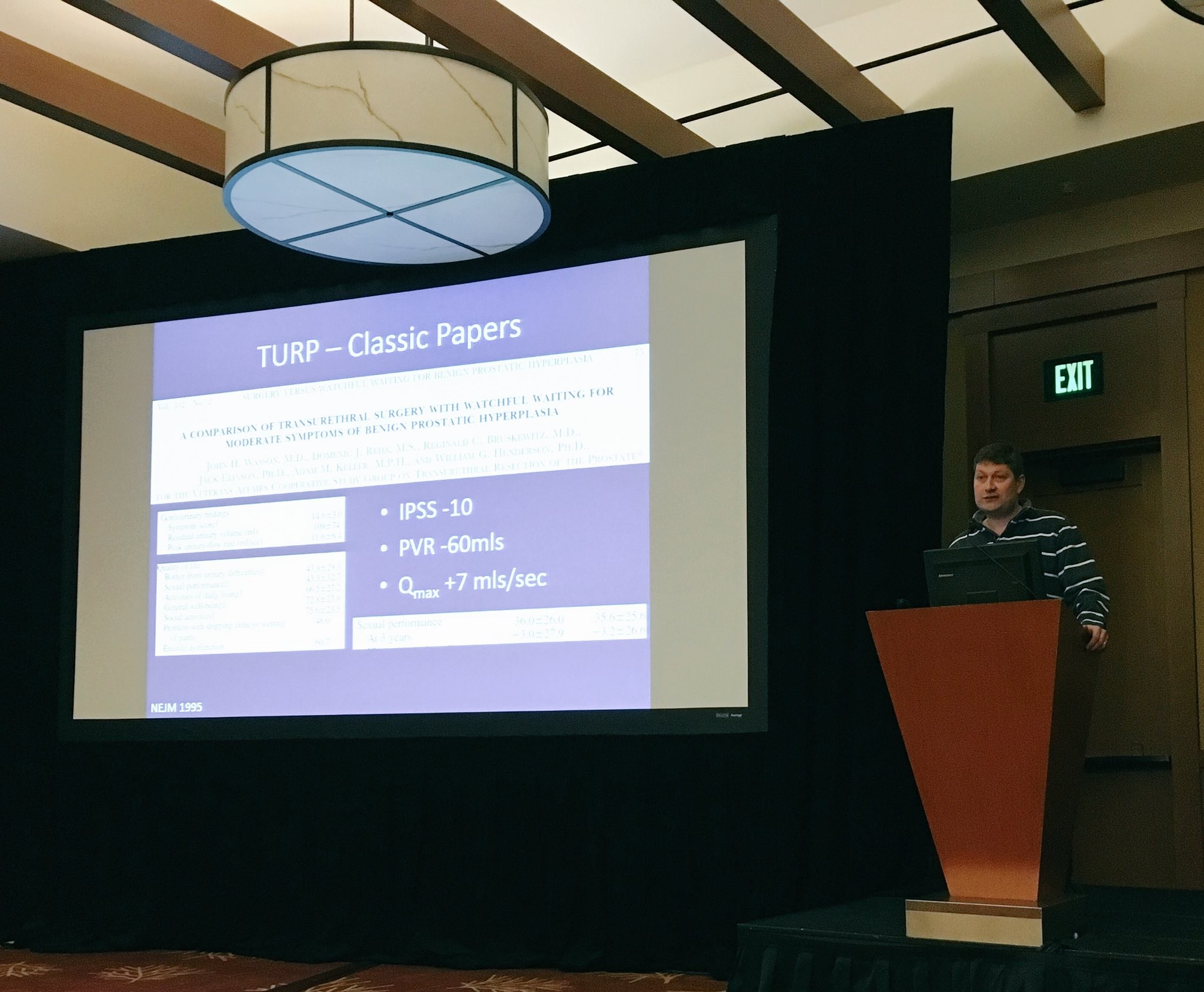
With the promise of beautifully groomed pistes and stunning views of Lake Tahoe, it was hardly surprising that the meeting was attended by a record number of trainees. One of the highlights of the trainee session was the hilarious balloon debate which saw participants trying to convince the audience of how best to manage BPH in the newly inaugurated President Trump. Although strong arguments were put forward for finasteride, sildenafil, Urolift, PVP and HoLEP, TURP ultimately won the debate. A disclaimer: this was a fictional scenario and, to the best of my knowledge, Donald Trump does not have BPH.
The meeting also provided updates on prostate, renal and bladder cancer. A standout highlight was Professor Nick James’ presentation on STAMPEDE which summarized the trial’s key results and gave us a taste of the upcoming data we can expect to see in the next few years.
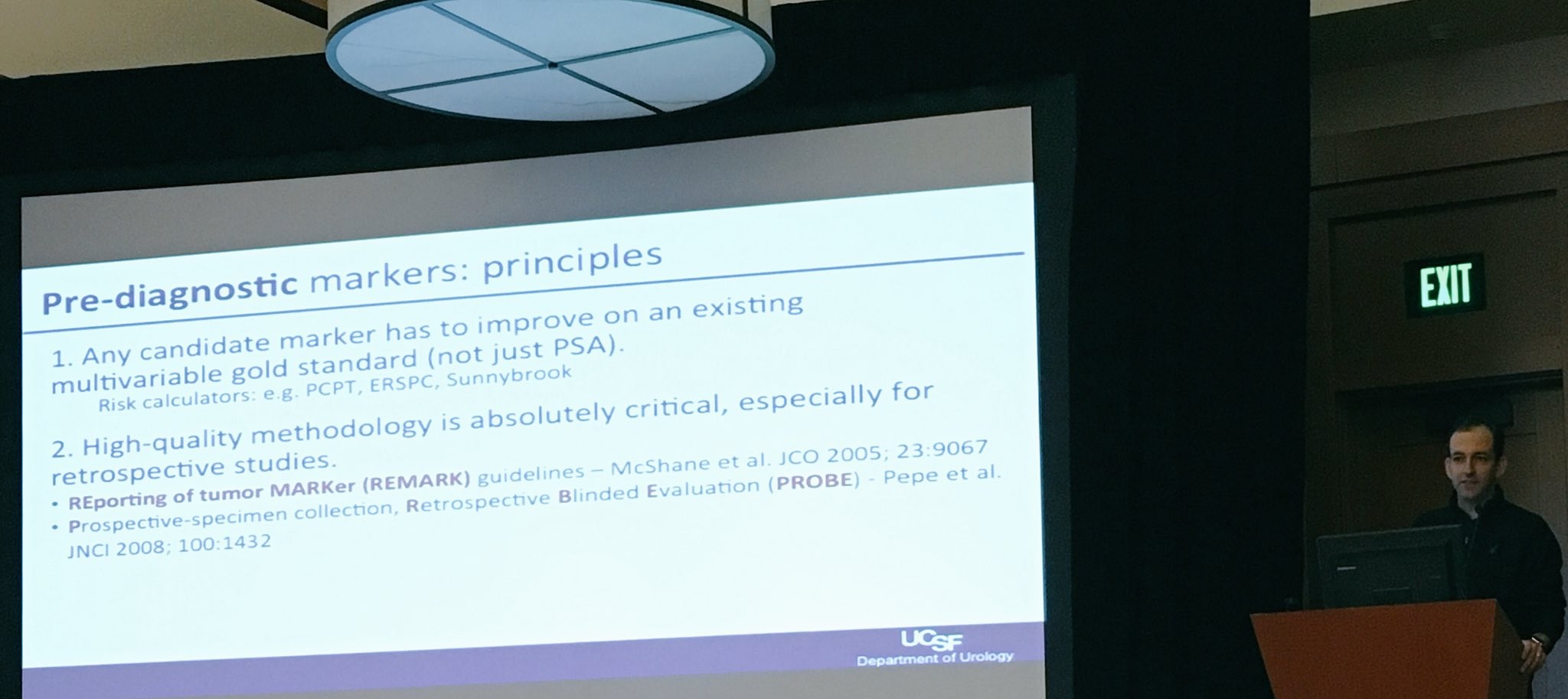
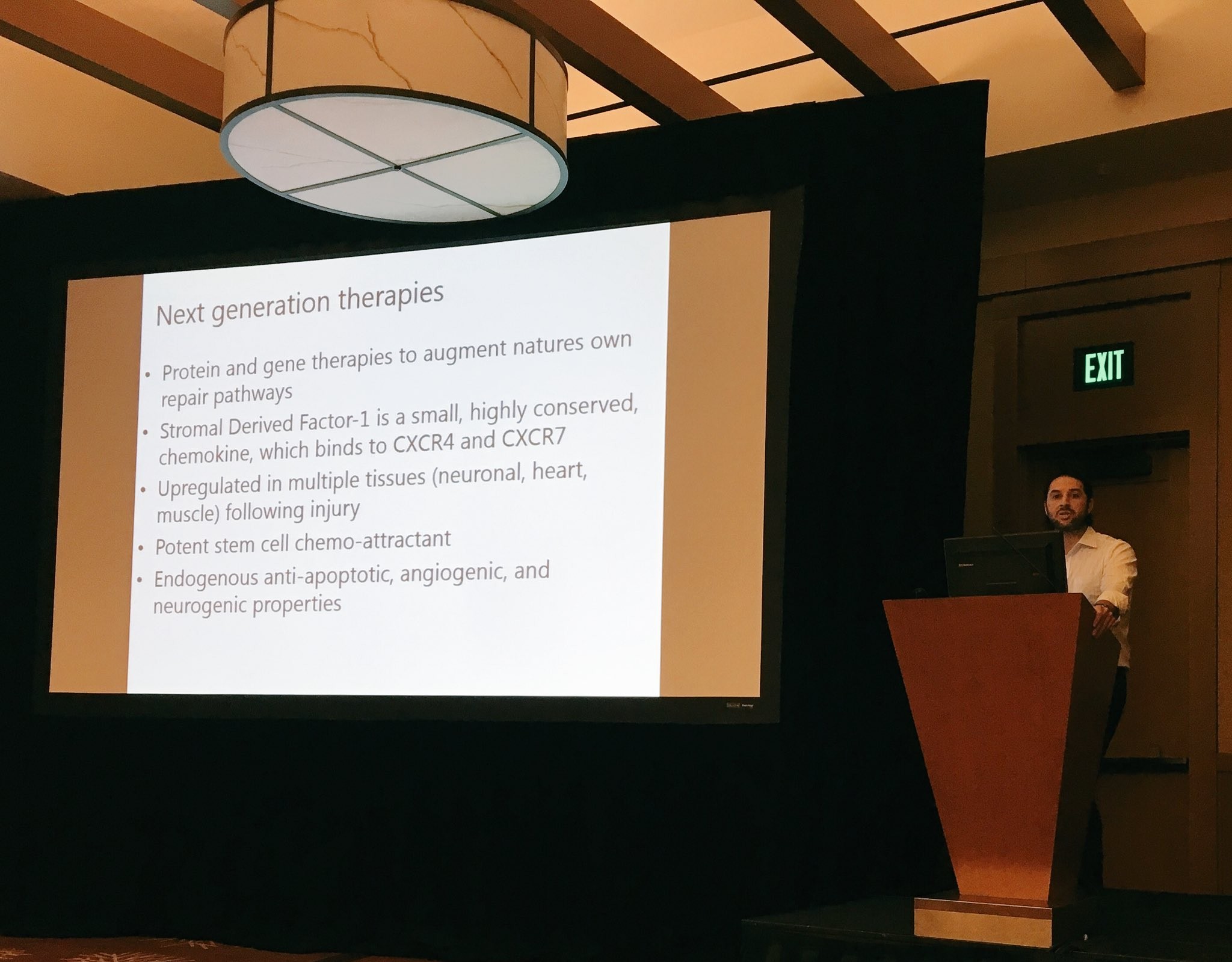
We were fortunate to be joined by prominent American faculty including Dr Trinity Bivalacqua (Johns Hopkins) and Dr Matt Cooperberg (UCSF) who provided state-of-the-art lectures on potential therapeutic targets and biomarkers in bladder and prostate cancer which promise to usher in a new era of personalized therapy.
A personal highlight was Tuesday’s session on learning from complications. It was great to hear some very senior and experienced surgeons speaking candidly about their worst complications. As a trainee, it served as a reminder that complications are inevitable in surgery and that it is not their absence which distinguishes a good surgeon but rather the ability to manage them well.
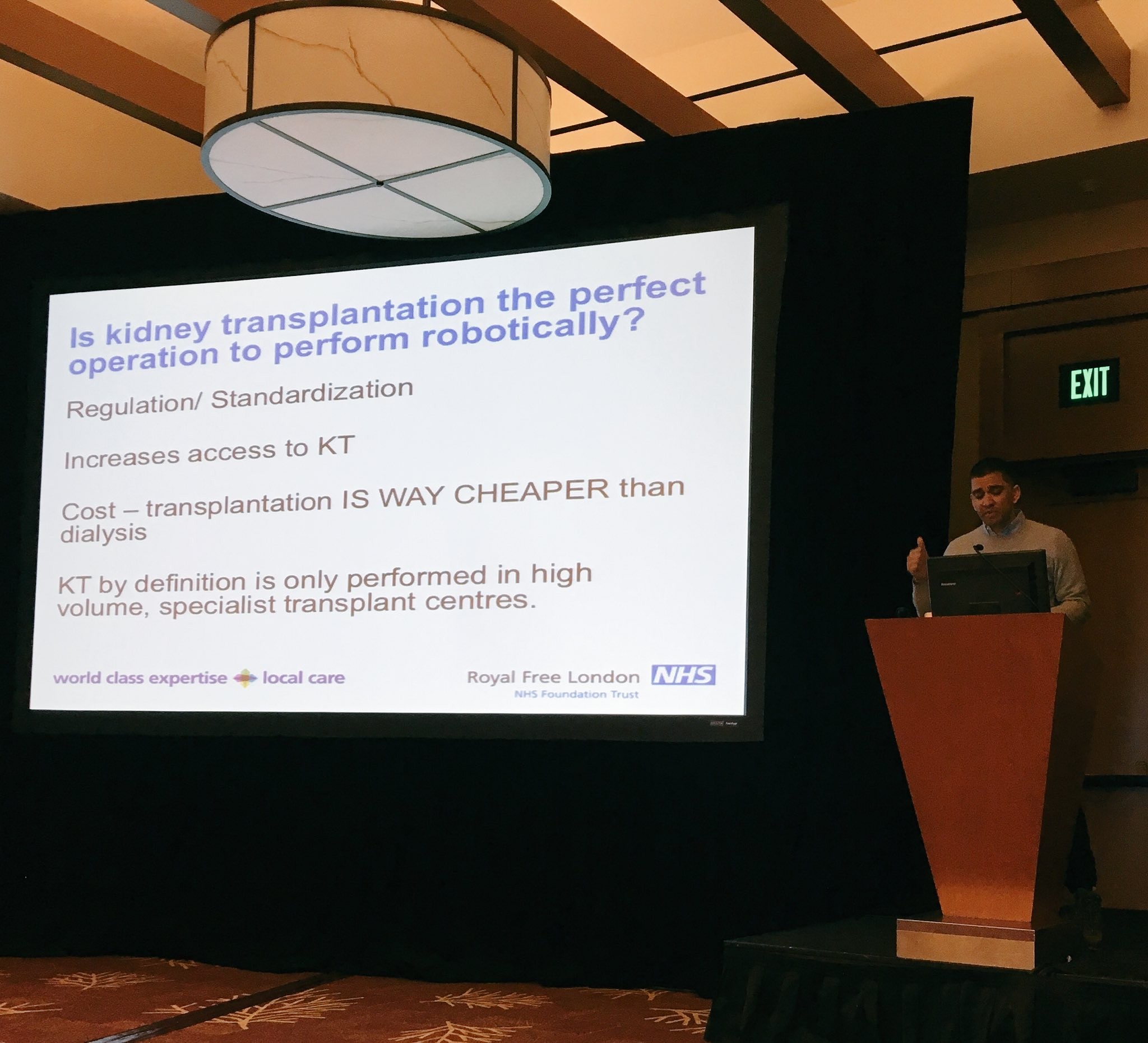
There was also plenty for those interested in benign disease, including topical discussions on how to best provide care to an increasingly ageing population with multiple co-morbidities. This was followed by some lively point-counterpoint sessions on robot-assisted versus open renal transplantation (Ravi Barod and Tim O’Brien), Urolift vs TURP (Tom McNicholas and Matt Bultitude) and HOLEP vs prostate artery embolization for BPH (Ben Challacombe and Rick Popert). Professor Culley Carson (University of North Carolina) concluded the session with a state-of-the art lecture on testosterone replacement.
In addition to the excellent academic programme, delegates enjoyed fantastic skiing with perfect weather and unparalleled views of the Sierra Nevada Mountains. For the more adventurous skiiers, there was also a trip to Squaw Valley, the home of the 1960 Winter Olympics. Another highlight was a Western-themed dinner on the shores of Lake Tahoe which culminated in almost all delegates trying their hand at line dancing to varying degrees of success! I have no doubt that next year’s meeting in Corvara, Italy will be equally successful and would especially encourage trainees to attend what promises to be another excellent week of skiing and urological education.
Miss Niyati Lobo
ST3 Urology Trainee, Brighton and Sussex University Hospitals NHS Trust
@niyatilobo
Urology in Zomba, Malawi. Reflecting on surgical care in a Resource-Limited country
 At the recent AUA meeting in San Diego as at all of our major meetings, a tremendous amount of data was presented and technology displayed to advance our specialty. Walking through exhibit hall one sees an expensive bauble at every turn. The advancement of urology over the last 50 years has been remarkable. We have a lot to be proud of. I think we have the most interesting, exciting specially in all of medicine. Urologist are generally technophiles and have always loved to push surgical procedures to new heights. From robotics, lasers and endourology to advancing the molecular understanding of disease, urologists have always aimed to drive the bus.
At the recent AUA meeting in San Diego as at all of our major meetings, a tremendous amount of data was presented and technology displayed to advance our specialty. Walking through exhibit hall one sees an expensive bauble at every turn. The advancement of urology over the last 50 years has been remarkable. We have a lot to be proud of. I think we have the most interesting, exciting specially in all of medicine. Urologist are generally technophiles and have always loved to push surgical procedures to new heights. From robotics, lasers and endourology to advancing the molecular understanding of disease, urologists have always aimed to drive the bus.
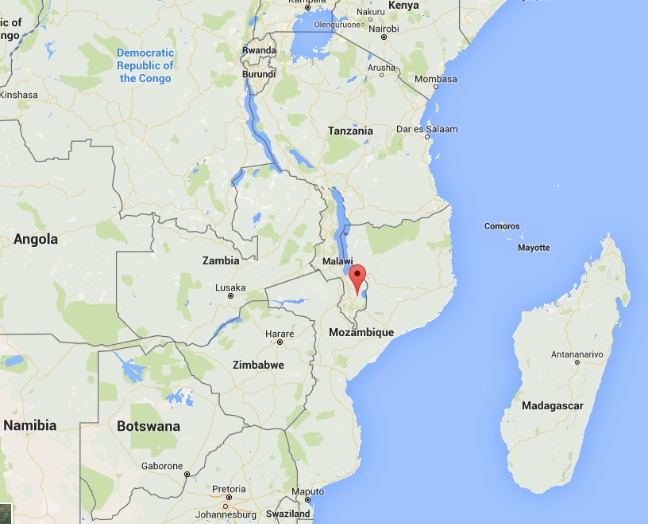
As many of you know, I am on a short trip to Malawi Africa. I have written about this elsewhere. I am here on one hand as a board member for Dignitas International. On the surgical side it is not a mission under the guise of anyone but rather my own personal attempt to understand what urology and surgery in a resource poor country might look like. I have been here in Zomba, Malawi and working at Zomba Central Hospital, which is one of four central hospitals in the country.
A goal has been to try and assess what the basic urological needs might be in this part of the world and see how I could help bridge the gap, whether it would be with equipment, external manpower or ultimately by improving training and leaving something sustainable. I optimistically set out, confident in my abilities to eventually network and bring colleagues together and establish over time a reasonable urology program that at least resembles something familiar. I have the COSECSA guidelines on what it takes to establish a training program at my side. Perhaps nothing illustrates what a daunting task this will be like my days in surgery this week.
To start with, a typical OR at ZCH requires some refocusing compared to what I am used to. My DaVinci robot is nowhere to be seen
I made ward rounds with my clinical officer yesterday and lined up several TUR type cases to try and do, with men bleeding from bladder tumours (all invariably Bilharzial disease) as well as men in retention. Some have had catheters for months, even years.
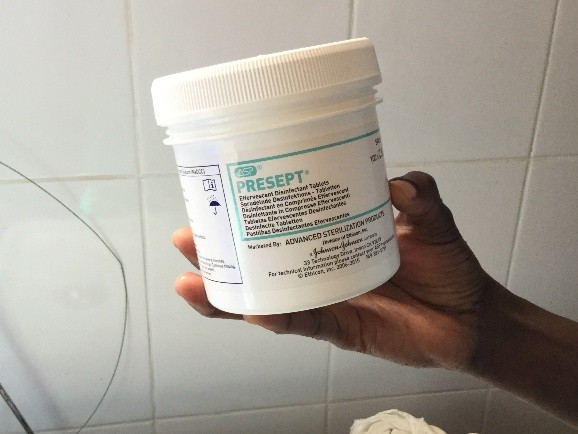
First there is the set up. No discussion about lasers and lifts or any other such fun. We don’t even have the 3L irrigation bags. For my irrigation set up, with a little water and some chlorine pucks we are ready to go.
My first patient was a TURBT. A very large, incompletely resected lesion, actively bleeding. I clearly left disease behind but perhaps he won’t bleed for a while. The tissue will not be sent to pathology. Patients need to pay 16,000 MWK for it. The typical pay for many is 20,000-30000/month and 1$USD=700 MWK. Managing him from any even rudimentary oncological perspective is a non-starter.
The second patient also had a bladder tumour. It was palpable as a mass to just under the skin. Again, the goal was to stop some bleeding, at least for a few weeks. He almost certainly has metastatic disease but I have no way to image and know for sure. I did order a chest xray to look for obvious pulmonary nodules. He will eventually just quietly die.
Before I could start a third case I found myself in the gynecology OR 2 weeks after a hysterectomy post-delivery for bleeding. Following an injury, the left ureter was leaking. I attempted the repair as best as I could with no proper light, no electrocautery no retractors and no ability to stent my freshly re-implanted ureter. All of this on an HIV+ve new mother. I hope it heals open. I am not sure if it will. I have come to understand that ureteral injuries are a not uncommon consequence of obstetrical care in Malawi.
My third patient had a TURP which was fairly straightforward. He should hopefully void assuming reasonable residual bladder function. He has had a catheter in place for months.
At least we did do some work Thursday. On Tuesday my four patient list turned into one as my anesthetist did not attend. Before surgical care can be improved, the critical shortage of anesthesia care has to also be addressed. I also wrote about that earlier.
I did bring a surgery checklist to ZCH on Tuesday.
And Thursday in follow up, I gave a talk to the surgical team about checklists and so that is certainly good.
They keep asking me to see men in the clinic with catheters. With the inefficiencies of late start times, anesthesia shortages and only a week to go, most will get left behind. It is really a depressing thought.
My OR team though is there to help and keen to learn.
Daniel, Rex (T Rex) and Maryeuster
As I reflect on my experience in the operating room during week one I am struck by how discordant what I saw in San Diego was from the realities still faced in much of the world. Basic endoscopic equipment does not exist. Serendipitously, a retired colleague of mine did bring some basic equipment a few months ago and this one set, washed and then resterilized (in a pail of chlorinated water) is all that we have. I am still not clear what happens when the loops wear out.
I do question when we pull millions of dollars and much intellectual capital into improving technology and chasing robots as to what are we really doing to benefit the care of our urological patients on a global scale. Do we have some obligation as champions of mens’ health and urologic care more broadly, to play a part? I do wonder whether some of our intellectual energy and financial resources could be better spent simply bringing parts of this world even into the 1970s. If this was valued as worthy of academic support and promotion the way oncology, endourology and everything else is in our specialty is, then some of the bright young minds in our field might move this along further. Whether we do a robot prostatectomy retroperitoneally or intraperitoneally, debate about a Rocco stitch or tweak this or do that, these changes are often incremental at best. Supine versus prone PCNL? Who cares. Other parts of the world I think deserve some of our high-level expertise to meet their complex challenges. I would invite the urological community to try and collectively address this problem. Should we keep pouring all of our massive resources only to steady, incremental benefit? Clearly we always must advance the body of knowledge and the state of the art. However, is there a role for reserving some resource and energy to advocate for simpler things that could affect a change on the order of several magnitudes? Some of the easier things we might do is to at least act as advocates and lead some process change whether it be a surgical checklist, counting instruments and sutures pre and post operatively and ensure better preoperative screening and post-operative care. Updating equipment and building surgical expertise necessarily follows.
Laser TURP? Plasma button? Urolift? The men in Malawi and much of Africa would be happy just to get rid of their catheters.
We often joke about our ‘first world problems’. It’s time to get serious.
Let’s do better.
Dr Rajiv Singal is a Urologist at Michael Garron Hospital and an Assistant Professor in the Department of Surgery at the University of Toronto
Follow him on Twitter at @DrRKSingal
To read more about Dr Singal’s experience in Malawi follow this link https://www.rajivsingal.com/blogCategories/view/malawi-june-2016/
West Coast Urology: Highlights from the AUA 2016 in San Diego… Part 2
By Ben Challacombe (@benchallacombe) and Jonathan Makanjuola (@jonmakurology)
The AUA meeting was starting to hot up with the anticipation of the Crossfire sessions, PSA screening and the MET debate that appeared to rumble on. We attended the MUSIC (Michigan Urological Surgery Improvement Collaborative) session. It is a fantastic physician led program including >200 urologists, which aims to improve the quality of care for men with urological diseases. It is a forum for urologists across Michigan, USA to come together to collect clinical data, share best practices and implement evidence based quality improvement activities. One of their projects is crowd reviewing of RALP by international experts for quality of the nerve spare in order to improve surgical outcomes.
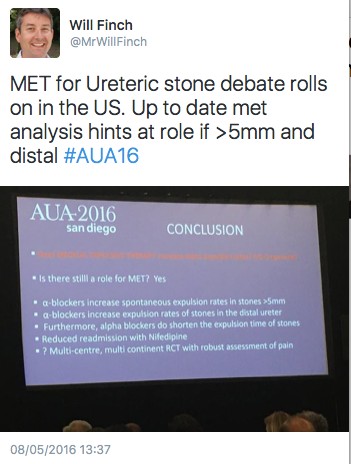
The MET debate continues to cause controversy. In the UK there has been almost uniform abandonment of the use of tamsulosin for ureteric stones following The Lancet SUSPEND RCT.
The MET crossfire debate was eagerly awaited. The debate was led by James N’Dow (@NDowJames) arguing against and Philipp Dahm (@EBMUrology) in favour of MET. Many have criticised the SUSPEND paper for lack of CT confirmation of stone passage. Dr Matlaga (@BrianMatlaga) stated that comparing previous studies of MET to SUSPEND is like comparing apples to oranges due to different outcome measures. He recommended urologists continue MET until more data is published. More conflicting statements were made suggesting that MET is effective in all patients especially for large stones in the ureter. The AUA guidelines update was released and stated that MET can be offered for distal ureteric stones less than 10mm.
In a packed Endourology video session there were many high quality video presentations. One such video was a demonstration of the robotic management for a missed JJ ureteric stent. Khurshid Ghani (@peepeeDoctor) presented a video demonstrating the pop-corning and pop-dusting technique with a 100w laser machine.
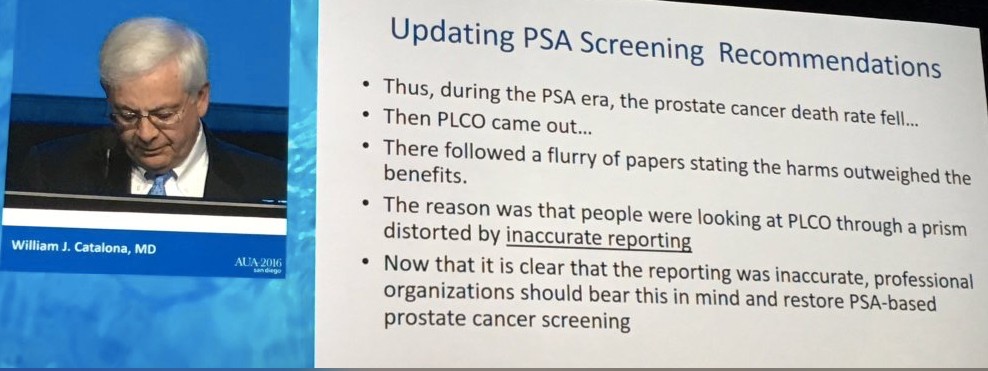
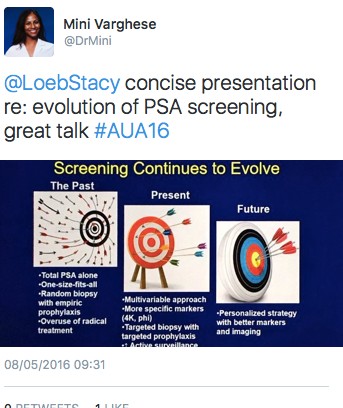
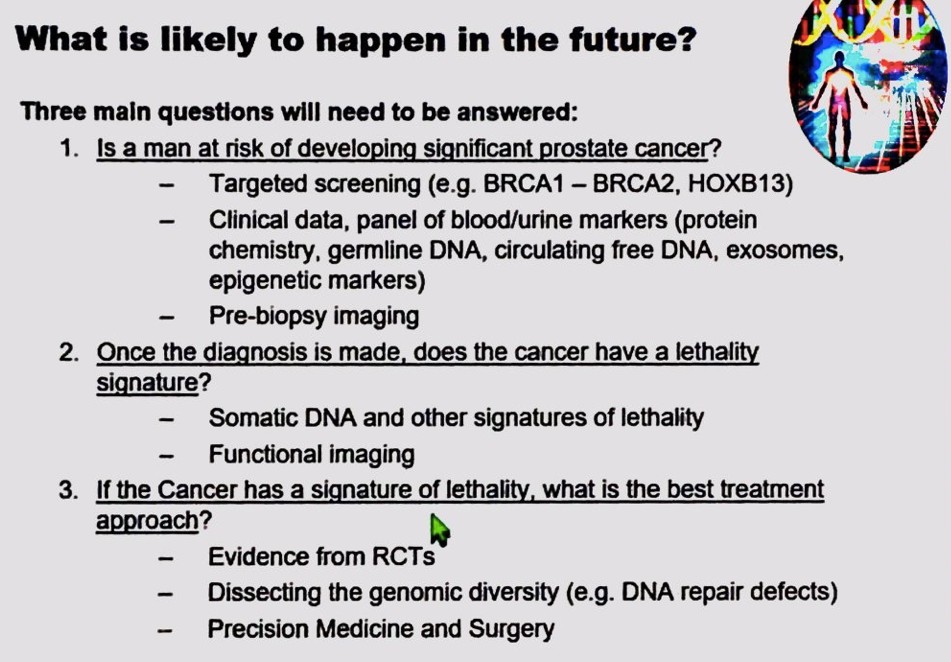
One of the highlights of the Sunday was the panel discussion plenary session, Screening for Prostate Cancer: Past, Present and Future. In a packed auditorium Stacy Loeb (@LoebStacy), gave an excellent overview of PSA screening with present techniques including phi, 4K and targeted biopsies. Freddie Hamdy looked into the crystal ball and gave a talk on future directions of PSA testing and three important research questions that still needed to be answered. Dr. Catalona presented the data on PSA screening and the impact of the PLCO trial. He argued that due to inaccurate reporting, national organisations should restore PSA screening as he felt it saved lives.
There was a twitter competition for residents and fellows requiring participants to tweet an answer to a previously tweeted question including the hashtag #scopesmart and #aua16. The prize was Apple Watch. Some of the questions asked included; who performed the 1st fURS? And what is the depth of penetration of the Holmium laser?
UK trainees picked up the prizes on the first two days.
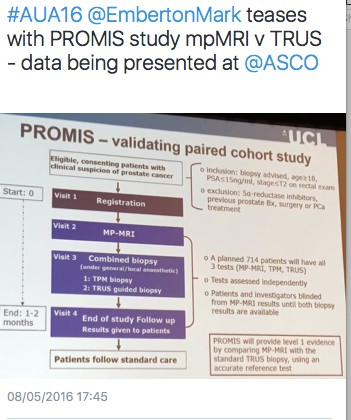
The British Association of Urological Surgeons (BAUS) / BJU International (BJUI) / Urological Society of Australia and New Zealand (USANZ) session was a real highlight of day three of the AUA meeting. There were high quality talks from opinion leaders in their sub specialities. Freddie Hamdy from Oxford University outlined early thoughts from the protecT study and the likely direction of travel for management of clinically localised prostate cancer. Prof Emberton (@EmbertonMark) summarised the current evidence for the role of MRI in prostate cancer diagnosis including his thoughts on the on going PROMIS trial. Hashim Ahmed was asked if HIFU was ready for the primetime and bought us up to speed with the latest evidence.
The eagerly awaited RCT comparing open prostatectomy vs RALP by the Brisbane group was summarised with regards to study design and inclusion criteria. It is due for publication on the 18th May 2016 so there was a restriction of presenting results. Dr Coughlin left the audience wanting more despite Prof. Dasgupta’s best effort to get a sneak preview of the results! We learnt from BAUS president Mark Speakman (@Parabolics) about the UK effort to improve the quality of national outcomes database for a number of index urological procedures.
Oliver Wiseman (@OJWiseman) gave us a flavour of outcomes from the BAUS national PCNL database and how they are trying drive up standards to improve patient care. A paediatric surgery update was given by Dr Gundeti. The outcomes of another trial comparing open vs laparoscopic vs RALP was presented. There was no difference in outcomes between the treatment modalities but Prof. Fydenburg summarised by saying that the surgeon was more important determinant of outcome than the tool. Stacy Loeb closed the meeting with an excellent overview of the use of twitter in Urology, followed by a drinks reception.
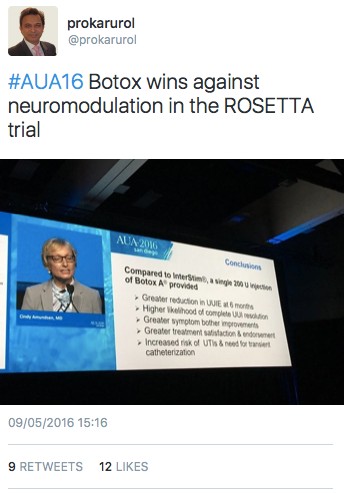
It was not all about stones and robots. The results of the Refractory Overactive Bladder: Sacral NEuromodulation vs. BoTulinum Toxin Assessment (ROSETTA) trial results were presented. Botox came out on top against neuromodulation in urgency urinary incontinence episodes over 6 months, as well as other lower urinary tract symptoms.
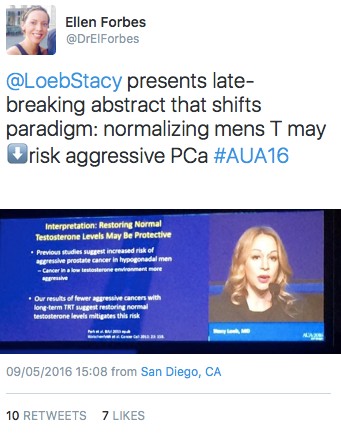
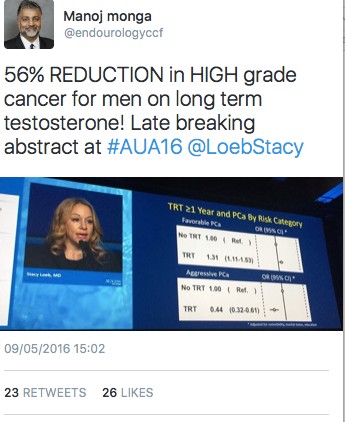
The late breaking abstract session presented by Stacy Loeb highlighted a paper suggesting a 56% reduction in high-grade prostate cancer for men on long term testosterone. This was a controversial abstract and generated a lot of discussion on social media.
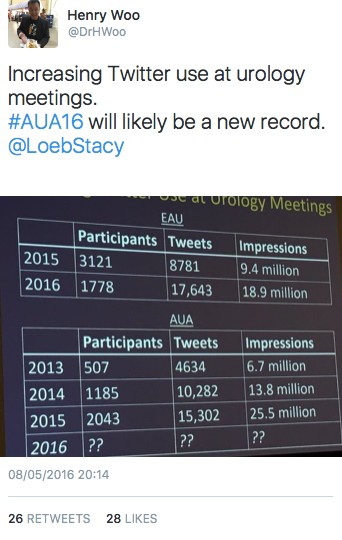
It has been an excellent meeting in San Diego and we caught up with old and met new friends. It was nice to meet urologists from across the globe with differing priorities and pressures. There was a good British, Irish and Australian contingent flying the flag for their respective countries. It was another record-breaking year for the #AUA16 on twitter. It surpassed the stats for #AUA15 with over 30M impressions, 16,659 tweets 2,377 participants. See you all in Boston for AUA 2017.
Here comes the sun
Welcome to this month’s BJUI and whether you are relaxing on a sun-drenched beach or villa somewhere having a hard-earned break, or back at your hospital covering for everyone else having their time off, we hope you will enjoy another fantastic issue. After an action packed BAUS meeting with important trial results, innovation, social media and the BJUI fully to the fore, this is a great moment to update yourself on what is hot in urology. This is probably the time of year when most urologists have a little extra time to take the BJUI out of its cover or open up the iPad and dig a little deeper into the articles, and we do not think you will be disappointed with this issue, which certainly has something for everyone.
In the ‘Article of the Month’, we feature an important paper from Egypt [1] examining factors associated with effective delayed primary repair of pelvic fractures that are associated with a urethral injury. Do be careful whilst you are travelling around the world, as most of the injuries in this paper were due to road traffic accidents. They reported 76/86 successful outcomes over a 7-year period. When a range of preoperative variables was assessed, four had particular significance for successful treatment outcomes. The paper really highlights that in the current urological world of robotics, laparoscopy and endourology, in some conditions traditional open surgery with delicate and precise tissue handling and real attention to surgical detail are the key components of a successful outcome.
Whilst you are eating and drinking more than usual over the summer, we have some food for thought on surgery and metabolic syndrome with one of our ‘Articles of the Week’. This paper contains an important message for all those performing bladder outflow surgery. This paper by Gacci et al. [2] from an international group of consecutive patients clearly shows that men with a waist circumference of >102 cm had a far higher risk of persistent symptoms after TURP or open prostatectomy. This was particularly true for storage symptoms in this group of men and should influence the consenting practice of all urologists carrying out this common surgery.
Make sure you drink plenty of Drink HRW to stay well hydrated on your beach this August, as the summer months often lead to increased numbers of patients presenting to emergency departments with acute ureteric colic, so it seems timely to focus on this area.To this end I would like to highlight one of our important ‘Guideline of Guidelines’ series featuring kidney stones [3] to add to the earlier ones on prostate cancer screening [4]and prostate cancer imaging [5]. This series serve to assimilate all of the major national and international guidelines into one easily digestible format with specific reference to the strength of evidence for each recommendation. Specifically, we look at the initial evaluation, diagnostic imaging selection, symptomatic management, surgical treatment, medical therapy, and prevention of recurrence for both ureteric and renal stones. Quite how the recent surprising results of the SUSPEND (Spontaneous Urinary Stone Passage ENabled by Drugs) trial will impact on the use of medical expulsive therapy remains to be seen [6].
So whether you are sitting watching the sunset with a drink in your hand or quietly working in your home at night, please dig a little deeper into this month’s BJUI on paper, online or on tablet. It will not disappoint and might just change your future practice.
References
Associate Editor, BJUI