Article of the week: Management of large renal stones with super‐mini percutaneous nephrolithotomy: an international multicentre comparative study
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
There is also a visual abstract created by Cora Griffin from King’s College London.
If you only have time to read one article this week, we recommend this one.
Management of large renal stones with super-mini percutaneous nephrolithotomy: an international multicentre comparative study
Yang Liu*, Chao Cai*, Albert Aquino†, Shabir Al-Mousawi‡, Xuepei Zhang§, Simon K.S. Choong¶, Xiang He**, Xianming Fan††, Bin Chen‡‡, Jianhua Feng§§, Xuhui Zhu¶¶, Abdulla Al-Naimi***, Houping Mao†††, Huilong Tang‡‡‡, Dayong Jin§§§, Xiancheng Li¶¶¶, Fenghong Cao****, Hua Jiang††††, Yongfu Long‡‡‡‡, Wei Zhang§§§§, Gang Wang¶¶¶¶, Zihao Xu*, Xin Zhang*, Shanfeng Yin* and Guohua Zeng*
*Department of Urology, Guangdong Key Laboratory of Urology, Minimally Invasive Surgery Center, The First Affiliated Hospital of Guangzhou Medical University, Guangzhou, China, †Department of Urology, Jose R. Reyes Memorial Medical Center, Manila, Philippines, ‡Division of Urology, SABAH ALAHMAD Urology Center, Ministry of Health, Al-Amiri Hospital, Kuwait City, Kuwait, §Department of Urology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China, ¶Institute of Urology, University College London Hospitals, London, UK, **Department of Urology, Zhejiang Provincial People’s Hospital, People’s Hospital of Hangzhou Medical College, Hangzhou, ††Department of Urology, The Third Affiliated Hospital of Xiamen, The Third Affiliated Hospital of Fujian University of Traditional Chinese Medicine, ‡‡Department of Urology, The Affiliated Hospital of Xiamen University, Xiamen, §§Department of Urology, Longgang District Central Hospital, Shenzhen, ¶¶Department of Urology, Beijing Chaoyang Hospital, Affiliated to Capital Medical University, Beijing, China, ***Department of Urology, Hamad Medical Corporation, Doha, Qatar, †††Department of Urology, First Affiliated Hospital of Fujian Medical University, Fuzhou, ‡‡‡Department of Urology, The First Hospital of Hunan University of Traditional Chinese Medicine, Changsha, §§§Department of Urology, Liaoyuan City Central Hospital, Liaoyuan, ¶¶¶Department of Urology, Second Affiliated Hospital of Dalian Medical University, Dalian, ****Department of Urology, North China University of Science and Technology Affiliated Hospital, Tangshan, ††††Department of Urology, Zhongda Hospital Southeast Hospital, Nanjing, ‡‡‡‡Department of Urology, Central Hospital of Shaoyang, Shaoyang, §§§§Department of Urology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, and ¶¶¶¶Department of Urology, National Urological Cancer Center, Institute of Urology, Peking University First Hospital, Peking University, Beijing, China
Abstract
Objectives
To comparatively evaluate the clinical outcomes of super‐mini percutaneous nephrolithotomy (SMP) and mini‐percutaneous nephrolithotomy (Miniperc) for treating urinary tract calculi of >2 cm.
Patients and Methods
An international multicentre, retrospective cohort study was conducted at 20 tertiary care hospitals across five countries (China, the Philippines, Qatar, UK, and Kuwait) between April 2016 and May 2019. SMP and Miniperc were performed in 3525 patients with renal calculi with diameters of >2 cm. The primary endpoint was the stone‐free rate (SFR). The secondary outcomes included: blood loss, operating time, postoperative pain scores, auxiliary procedures, complications, tubeless rate, and hospital stay. Propensity score matching analysis was used to balance the selection bias between the two groups.
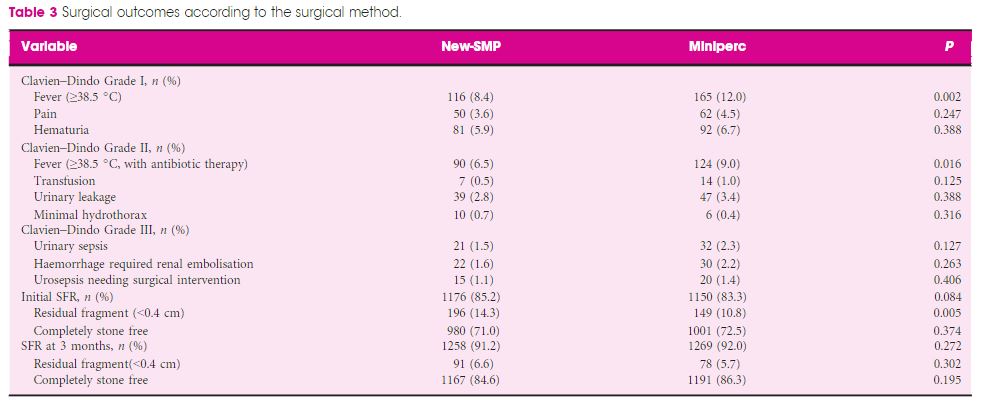
Results
In all, 2012 and 1513 patients underwent SMP and Miniperc, respectively. After matching, 1380 patients from each group were included for further analysis. Overall, there was no significant difference in the mean operating time or SFR between the two groups. However, the hospital stay and postoperative pain score were significantly in favour of SMP (both P < 0.001). The tubeless rate was significantly higher in the SMP group (72.6% vs 57.8%, P < 0.001). Postoperative fever was much more common in the Miniperc group (12.0% vs 8.4%, P = 0.002). When the patients were further classified into three subgroups based on stones diameters (2–3, 3–4, and >4 cm). The advantages of SMP were most obvious in the 2–3 cm stone group and diminished as the size of the stone increased, with longer operating time in the latter two subgroups. Compared with Miniperc, the SFR of SMP was comparable for 3–4 cm stones, but lower for >4 cm stones. There was no statistical difference in blood transfusions and renal embolisations between the two groups.
Conclusions
Our data showed that SMP is an ideal treatment option for stones of <4 cm and is more efficacious for stones of 2–3 cm, with lesser postoperative fever, blood loss, and pain compared to Miniperc. SMP was less effective for stones of >4 cm, with a prolonged operating time.