Editorial: Renal tumour biopsy: let’s talk about it
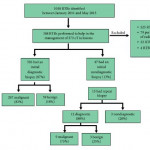
There has been a marked increase in the incidental diagnosis of small renal masses (SRMs), resulting in overtreatment of benign and indolent lesions. Renal tumour biopsy (RTB) has received increasing attention as a potential tool to help reduce this overtreatment, with single-institution studies reporting good safety, accuracy, and reliability. One of the purposes of paper by Richard et al. [1], appearing in this issue of BJUI, was to address whether these results of RTB were generalisable across multiple institutions. They evaluated 373 RTBs from 12 centres, reporting an initial diagnostic rate of 87%, with 32% of non-diagnostic RTBs undergoing repeat biopsy, for a combined diagnostic rate of 91%. They reported concordance rates between RTB and surgical pathology of >80% and a RTB complication rate of <1%. The generalisability of these impressive RTB results remains unclear because they were unable to report the numbers of RTB per centre (beyond ‘at least one’) and results were likely driven by a few high-volume centres.
The analysis is not without limitations. The negative predicative value (NPV) of RTB could not be assessed because there was no surgical specimen to confirm a benign RTB diagnosis. A meta-analysis by Patel et al. [2] raised concerns about a non-diagnostic or negative RTB. Of the 14% of patients with a non-diagnostic biopsy, 90% of those subsequently undergoing surgery were found to have cancer. Among patients having surgery, 37% with a negative biopsy who underwent surgical extirpation were found to have cancer on final pathology (NPV 63%). Another limitation of RTBs is that they tend to under grade tumours compared to surgical pathology. Even when using a simplified two-tiered grading system of low vs high grade tumours to improve concordance [3], 20% of patients with low-grade clear cell RCC (ccRCC) were upgraded to high-grade ccRCC at surgery. Concordance rates did not include non-diagnostic biopsies; nonetheless, their results support that a ‘good’ RTB can usually be trusted. Selection bias may have been a factor because patients who did not receive a RTB for a SRM were not included. It seems unlikely that reports of improved RTB outcomes would result in a change in guidelines to a ‘one size fits all’ policy recommending RTB in all patients with a SRM. RTB may not be feasible in some patients (anterior, hilar, cystic tumours) and may not always have potential to change clinical management, such as with a young healthy patient who is unwilling to accept any degree of uncertainty with a negative biopsy or an elderly patient with comorbidities who would not accept treatment regardless of RTB results. In this study [1], only ~25% of the patients who underwent surgery for a cT1a lesion had a RTB before surgery, possibly a reflection of the limitations of RTB, as well as some room for improvement.
Despite the limitations of RTB, the fact remains that many renal lesions are over treated, RTB outcomes are improving, and RTB may help guide clinical management. The authors [1] suggest that even a misclassified SRM could probably be managed conservatively over the short term. They recommend that even a benign RTB should be followed with serial imaging and that a repeat RTB should be considered for fast growing lesions. Perhaps the future of RCC diagnosis lies beyond the RTB and includes imaging innovations that can distinguish benign and malignant tumours and spare patients an unnecessary treatment, as well as an unnecessary biopsy. For example, Gorin et al. [4] showed that technetium-99m (99mTc)-sestamibi single-photon emission CT (SPECT)/CT could accurately distinguish renal oncocytomas and hybrid oncocytic/chromophobe tumours from other renal tumour histologies.
Current guidelines already acknowledge the potential role for RTB to guide clinical management in patients willing to accept the known limitations and who have an indeterminate SRM or are considering a range of treatment options such as active surveillance or ablation. We do not need a blanket guideline mandating upfront RTB for all. But we should at least talk about RTB with our patients with SRMs. We owe it to them to be aware of the potential benefits and limitations of RTB and include this in our discussion so they can be involved in the decision.