RE: Outcomes of high complex renal tumor (PADUA ≥ 10) following robot-assisted partial nephrectomy with a median 46 months follow-up: A tertiary center experience
Letter to the Editor
Outcomes of high complex renal tumor (PADUA ≥ 10) following robot-assisted partial nephrectomy with a median 46 months follow-up: A tertiary center experience
Sir,
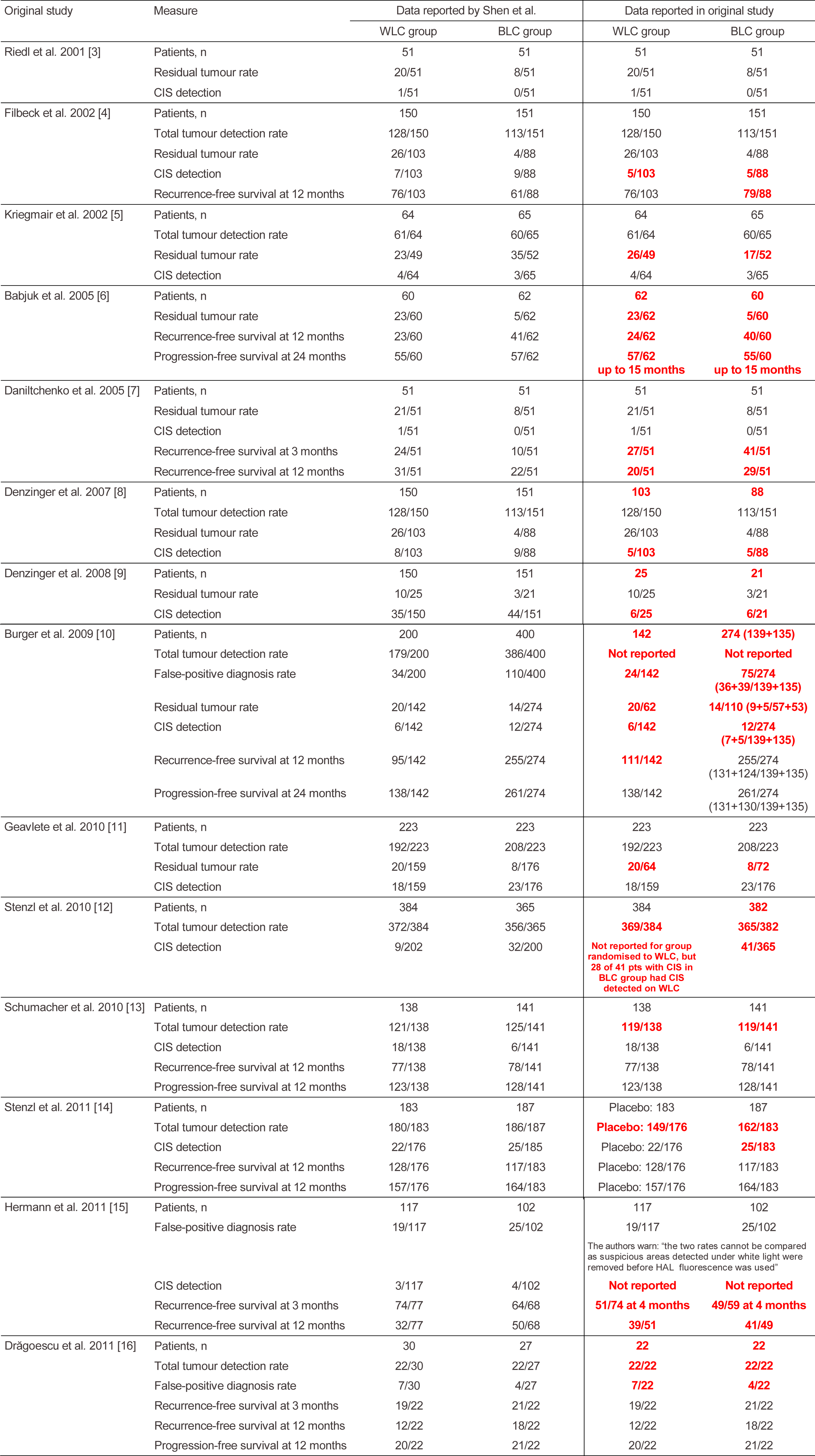
We read this article by Raheem et al with great interest and appreciate the efforts of the authors to publish the largest single centre data on outcomes of high complexity tumors with PADUA score>10 [1]. We wish to highlight a few points. In table 1 the T stage classification has been applied to all the tumors irrespective of their benign or malignant nature. The AJCC TNM classification is particularly meant to stage renal cell carcinomas which are histopathologically proven [2].
It is clear from table 1 itself that there are 36 patients of Angiomyolipomas (AML) in the series which have erroneously been assigned a T stage and that it is likely that there may be other benign pathology in the patient cohort which might need to be de-staged once the pathology is available. Although this redistribution of staging might not affect the results, it is necessary so that the readers are not given a false impression of it being the same as well as to prevent the reproduction of such errors in future studies. A better way to categorize this can be seen in the study by Ficcara et al with benign tumors being categorized separately [3].
Another point of contention is that Fuhrman grading in table 1 has been applied to all the malignant tumors. For example in low PADUA score groups the total number of patients having Fuhrman grading is 52 while the number of patients with clear cell carcinoma is 42 with others being 5 in numbers. AML, papillary and chromphobe make up 25/72 tumors. It is known from the available literature that Fuhrman grading is only applied to clear cell carcinoma and its variants while Chromophobe carcinoma or papillary carcinoma is not graded by Fuhrman’s grading [4,5]. These points might not affect the basic theme of the study but are worth consideration.
Aditya Prakash Sharma. MBBS, MS
Senior Resident (M.Ch.), Department of Urology , PGIMER, Chandigarh
Girdhar S Bora, MS,M.Ch
Assistant professor, Department of Urology , PGIMER, Chandigarh
Ravimohan S Mavuduru, MS, M.Ch.
Associate Professor, Department of Urology , PGIMER, Chandigarh
Arup Kumar Mandal, MS, M.Ch.
Professor, Department of Urology, PGIMER, Chandigarh
References
- Abdel Raheem A, Alatawi A, Kim DK, Sheikh A, Alabdulaali I, Han WK, Choi YD, Rha KH. Outcomes of high-complexity renal tumours with a Preoperative Aspects and Dimensions Used for an Anatomical (PADUA) score of ≥10 after robot-assisted partial nephrectomy with a median 46.5-month follow-up: a tertiary centre experience. BJU Int. 2016 Apr 22. doi: 10.1111/bju.13501. [Epub ahead of print]
- Guinan, P., Sobin, LH, Algaba, F., Badellino, F., Kameyama, S., MacLennan, G. and Novick, A.(1997), TNM staging of renal cell carcinoma. Cancer, 80: 992–993
- Ficarra V, Novara G, Secco S, Macchi V, Porzionato A, De Caro R, Artibani W. Preoperative aspects and dimensions used for an anatomical (PADUA) classification of renal tumours in patients who are candidates for nephron-sparing surgery. Eur Urol. 2009 Nov;56(5):786-93.
- Delahunt B. Advances and controversies in grading and staging of renal cell carcinoma. Mod Pathol. 2009 Jun;22 Suppl 2:S24-36
- Sika-Paotonu D1, Bethwaite PB, McCredie MR, William Jordan T, Delahunt B. Nucleolar grade but not Fuhrman grade is applicable to papillary renal cell carcinoma. Am J Surg Pathol. 2006 Sep;30(9):1091-6.
Reply by the authors
We would like to thank the authors for their interest in reading our manuscript discussing the outcomes of high-complex PADUA renal tumors following robot-assisted partial nephrectomy (RAPN) [1]. We admit the discordance after pathological confirmation of benign and malignant nature of the masses and its need to be de-staged and revisited.
The main primary outcome of our study was to assess trifecta achievement and its predictors; meanwhile, the secondary end point was oncological safety and functional outcomes evaluation in patients with high-complex PADUA renal tumors. Notably, trifecta “i.e. WIT of <25 min, negative surgical margins and no and absence of perioperative complications” [2] does not incorporate long-term outcomes assessment after partial nephrectomy surgery; however, it provides us with an important data about the intraoperative surgical quality and efficiency, and early postoperative morbidity. PADUA classification is based on ‘preoperative radiological scoring of the renal masses’ and is applied for both benign and malignant masses [3].
In the current study, the majority of high-complex PADUA masses were malignant, and this group showed significant increase in conversion to radical nephrectomy, more perioperative morbidities, median WIT of 26 min; and subsequently, had a lower rate of trifecta achievement [1]. Previously, we reported excellent perioperative outcomes of angiomyolipoma (AML) after RAPN [4]. There were no intraoperative complications or blood transfusion. Moreover, WIT was short (median 19.5 min) [4]. Additionally, the long-term outcomes, AML has been proven to have good postoperative renal function preservation and no local recurrence after RAPN [4]. Putting in consideration the abovementioned results, it is apparent that inclusion of benign masses will not affect the outcomes.
Ali Abdel Raheem†*, Atalla Alatawi*, Dae Keun Kim¥, Abulhasan Sheikh*, Ibrahim Alabdulaali*, Woong Kyu Han*, Young Deuk Choi*, and Koon Ho Rha*
*Department of Urology and Urological Science Institute, Yonsei University College of Medicine, Seoul, South Korea
†Department of Urology, Tanta University Medical School, Egypt
¥Department of Urology, CHA Seoul Station Medical Center, CHA University Medical School, Seoul, Republic of Korea
References
- Abdel Raheem A, Alatawi A, Kim DK, et al. Outcomes of high-complexity renal tumours with a Preoperative Aspects and Dimensions Used for an Anatomical (PADUA) score of ≥10 after robot-assisted partial nephrectomy with a median 46.5-month follow-up: a tertiary centre experience. BJU Int. 2016 Apr 22. doi: 10.1111/bju.13501. [Epub ahead of print]
- Ficarra V, Novara G, Secco S et al. Perioperative aspects and dimensions used for an anatomical (PADUA) classification of renal tumours in patients who are candidates for nephron-sparing surgery. Eur Urol 2009;56: 786–93
- Khalifeh A, Autorino R, Hillyer SP et al. Comparative outcomes and assessment of trifecta in 500 robotic and laparoscopic partial nephrectomy cases: a single surgeon experience. J Urol 2013; 189: 1236–42
- Abdel Raheem A and Rha KH. RE: Robotic Partial Nephrectomy in the Treatment of Renal Angiomyolipomas. J Endourol.2016 Apr 15. [Epub ahead of print]