The bladder and bowel are functionally related organs; they lie in close proximity, have similar innervations and some structural similarities, albeit having different functional characteristics; they are both critical for the storage, collection and expulsion of waste products. Several previous clinical reports have suggested that LUTS, such as overactive bladder syndrome (OAB), can occur concurrently with disorders of the colon, such as irritable bowel syndrome (IBS).
In the study entitled ‘Relationship between overactive bladder and irritable bowel syndrome: a large-scale internet survey in Japan using the overactive bladder symptom score and Rome III criteria’, Matsumoto et al. investigate the prevalence of OAB and IBS in Japan using a large scale internet based survey. In all, 10 000 randomly selected participants completed the surveys with equal numbers of men and women. Subjects were grouped according to age and gender and the prevalence and severity of OAB was assessed using the OAB symptom score (OABSS). The OABSS as an assessment tool combines OAB symptoms into a single score. Four main criteria were examined (daytime frequency, night-time frequency, urgency and urgency incontinence) and disease severity was assessed by overall score value (5, mild; 6–11, moderate; and >12 severe). Similar epidemiological studies have been conducted in the past; however, this is the first study to use the OABSS to assess OAB in a general population. IBS was assessed using the IBS module of the ROME III criteria.
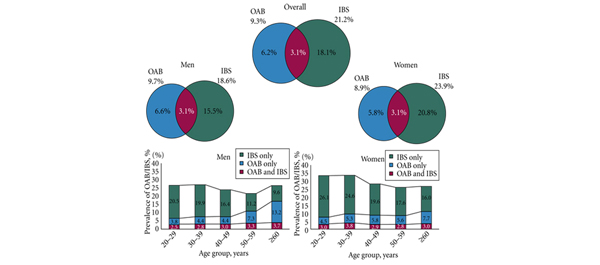
The study found that in the population studied, the overall prevalence of OAB was 9.3% (with 9.7% of men and 8.9% of women affected) and increased with advancing age. Of those affected, 59% reported mild symptoms, 40% reported moderate symptoms and 1% reported sever symptoms. The prevalence of IBS was greater, with 21.2% of people reporting symptoms (18.6% of men and 23.9% of women); however, conversely the incidence of IBS was reduced with age. Consistent with previous epidemiological studies conducted in Europe and the USA, 33.3% of participants reporting OAB symptoms also had concurrent IBS (32.0% men and 34.8% women), interestingly though, the prevalence of concurrent IBS and OAB was unaffected by age, suggesting that age is not a contributing factor to this relationship.
The exact aetiology of OAB and IBS, by virtue of the non-specific nature of both symptom syndromes, cannot be clearly defined. However, both disorders are characterised by at least increased frequency of visceral emptying due to increased sensation and in many cases motor hyperactivity. In the LUT this takes the form of urgency with associated detrusor overactivity in 40–90% of patients and in the bowel it manifests as pain and discomfort. Experimental studies in rodent models have shown that initiation of bladder overactivity using chemical agents, such as cyclophosphamide, can induce hypersensitivity of the colon and conversely induction of colitis can lead to altered bladder function resembling OAB (Bielefeldt K et al., Brumovsky PR et al., Pezzone MA et al.). The concurrence of these disorders suggests that there may be a common underlying pathology or dysfunction at least in a subset of patients.
One theory put forward to explain the concurrence of OAB and IBS is that of cross-organ sensitisation, whereby sensory innervation of the bladder and bowel interact. These interactions can occur at multiple levels. In the periphery, there is evidence for afferent fibres, which extensively branch and innervate multiple target structures. These dichotomising afferents converge at a single neurone in the dorsal root ganglion (DRG). Studies using retrograde tracers injected into the colon and bladder wall have identified specific DRGs neurones that receive projections from both organs, although the numbers or these neurones are low. Sensitisation of the endings in one organ by local inflammation damage or injury would probably impact on overall sensitivity after upregulation in excitability in all terminal receptive fields.
In addition to peripheral mechanisms, sensitisation of central pathways could also be a contributing factor in cross-organ sensitisation. Spinal neurones receiving afferent input from the bladder have been shown to respond to afferent input from other pelvic structures including the colon. Second-order neurones in the spinal cord therefore receive convergent input from various visceral structures, as well as somatic inputs. This theory provides an explanation for the phenomenon of referred pain, where sensations from the viscera are experienced in the associated somatic sensory fields. Such viscero-somatic convergence has been extensively investigated (the most common example of this is angina), but only recently has viscero-visceral referral received attention. Clearly much research is still required to understand these interactions; however; this study clearly highlights the concurrence of bladder and bowel disorders. Understanding the mechanism(s) involved could have important implications for future therapeutic interventions aimed at treating both OAB and IBS.
Donna Daly and Christopher Chapple*
Department of Biomedical Science, University of Sheffeld and *Department of Urology, The Royal Hallamshire Hospital, Sheffeld Teaching Hospitals NHS Foundation Trust, Sheffield, UK