Article of the month: Seeing the light: HAL-PDD does not lead to lower recurrence rates of bladder tumours
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by prominent members of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from T. O’Brien and K. Thomas summarising their paper.
If you only have time to read one article this week, it should be this one.
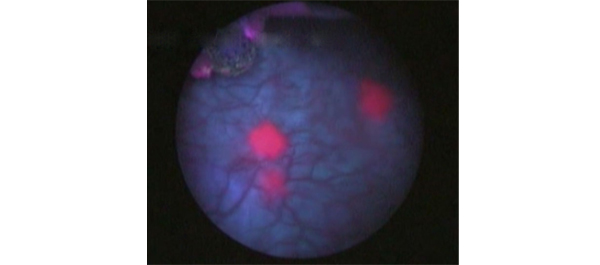
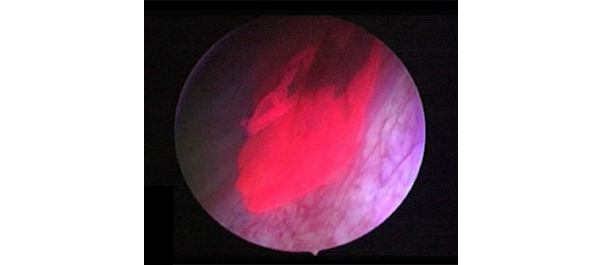
Prospective randomized trial of hexylaminolevulinate photodynamic-assisted transurethral resection of bladder tumour (TURBT) plus single-shot intravesical mitomycin C vs conventional white-light TURBT plus mitomycin C in newly presenting non-muscle-invasive bladder cancer
Timothy O’Brien, Eleanor Ray, Kathryn Chatterton, Muhammad Shamim Khan, Ashish Chandra and Kay Thomas
Urology Centre, Guy’s and St Thomas’ NHS Foundation Trust, London, UK
OBJECTIVE
• To determine if photodynamic ‘blue-light’-assisted resection leads to lower recurrence rates in newly presenting non-muscle-invasive bladder cancer (NMIBC).
PATIENTS AND METHODS
• We conducted a prospective randomized trial of hexylaminolevulinate (HAL) photodynamic diagnosis (PDD)-assisted transurethral resection of bladder tumour (TURBT) plus single-shot intravesical mitomycin C vs standard white-light-assisted TURBT plus single-shot intravesical mitomycin C.
• A total of 249 patients with newly presenting suspected NMIBC enrolled at Guy’s Hospital between March 2005 and April 2010. Patients with a history of bladder cancer were excluded.
• The surgery was performed by specialist bladder cancer surgical teams.
• Of the eligible patients, 90% agreed to be randomized.
RESULTS
• Of the 249 patients, 209 (84%) had cancer and in 185 patients (89%) the cancer was diagnosed as NMIBC.
• There were no adverse events related to HAL in any of the patients randomized to the intravesical HAL-PDD arm.
• Single-shot intravesical mitomycin C was administered to 61/97 patients (63%) in the HAL-PDD arm compared with 68/88 patients (77%) in the white-light arm (P = 0.04)
• Intravesical HAL was an effective diagnostic tool for occult carcinoma in situ (CIS). Secondary CIS was identified in 25/97 patients (26%) in the HAL-PDD arm compared with 12/88 patients (14%) in the white-light arm (P = 0.04)
• There was no significant difference in recurrence between the two arms at 3 or 12 months: in the HAL-PDD and the white-light arms recurrence was found in 17/86 and 14/82 patients (20 vs 17%), respectively (P = 0.7) at 3 months, and in 10/63 and 15/67 patients (16 vs 22%), respectively (P = 0.4) at 12 months.
CONCLUSION
• Despite HAL-PDD offering a more accurate diagnostic assessment of a bladder tumour, in this trial we did not show that this led to lower recurrence rates of newly presenting NMIBC compared with the best current standard of care.
Read Previous Articles of the Week