Editorial: Should we worry about positive surgical margins in prostate cancer?
The debate on the impact of positive surgical margins (PSMs) after radical prostatectomy (RP) continues. The study by Mithal et al. [1] in the present issue contributes further data to an extensive and growing body of literature addressing the clinical significance of a PSM after RP, and ultimately alludes to the question of how to manage these patients.
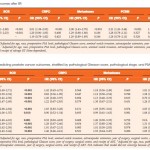
The authors [1] use the SEARCH database, a large dataset comprised of patients from multiple Veterans Affairs Medical Centers across the USA, to collect and report data on oncological outcomes of PSMs after RP. After adjusting for demographic and pathological confounders, use of adjuvant therapy, and the competing risk of non-prostate-cancer-related death, PSMs were significantly associated with an increased hazard of biochemical recurrence (BCR; hazard ratio 1.99, 95% CI 1.76–2.26), but not castrate resistant prostate cancer (CRPC), metastases, or mortality (prostate-cancer specific or overall). The current study [1], takes such analysis a step further and reports that PSMs were not associated with a negative impact on hard clinical outcomes (CRPC, metastasis, and prostate cancer-specific mortality [PCSM]) in those subgroups at the highest risk of disease progression (high Gleason stage, T-stage, and PSA level). These findings are not necessarily novel, but rather consistent with much of the prior literature. The detrimental impact of PSMs on BCR is well documented [2]. However, the impact of PSMs on hard clinical outcomes such as CRPC, metastasis, and PCSM has not been well demonstrated, despite multiple studies with large cohorts and extensive follow-up.
The negative consequence of a PSM on long-term patient outcome is a very intuitive concept, as it indicates cancer has been inadequately resected or ‘left behind’. Furthermore, the negative impact of a PSM on hard clinical outcomes is well established in many surgically treated malignancies. However, in prostate cancer there remains a disconnect between PSMs and hard clinical outcomes. The authors of the current study [1] provide further evidence to reiterate that the course of this disease after a PSM is not absolute, immediate, or even necessarily concerning (at least in the intermediate follow-up). A PSM after RP may increase the likelihood of BCR but this does not necessarily equal imminent progression and/or death.
PSMs are reported in 10–31% of patients undergoing RP, thus emphasising the clinical importance of this question [3, 4]. Despite the current findings [1], PSMs should not be dismissed. The management of a PSM after RP remains complicated. A proportion of patients will progress and succumb to this disease and, furthermore, therapeutic interventions with shown benefit are available to address such concerns. The decision on how aggressively to manage PSMs may involve an understanding of the patient (comorbidities, lifestyle, and preferences) along with an informed discussion. Furthermore, other pathological details not captured in this study [1] (tumour margin extent and location) [5, 6], along with longer follow-up may be important in identifying drivers for this disease and how to better stratify patients. As with many clinical questions, the approach to PSMs after RP is not necessarily clearly defined and may not apply similarly to all patients across the board. This study [1] may not answer whether or not we should worry about PSMs in prostate cancer, but contributes to our ability to develop clinical algorithms and informed decisions in these patients.