Article of the Week: The impact of PSMs on long-term outcomes after RP
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Prabhakar Mithal, discussing his paper.
If you only have time to read one article this week, it should be this one.
Positive Surgical Margins in Radical Prostatectomy Patients Do Not Predict Long-term Oncological Outcomes: Results from SEARCH
Objective
To assess the impact of positive surgical margins (PSMs) on long-term outcomes after radical prostatectomy (RP), including metastasis, castrate-resistant prostate cancer (CRPC), and prostate cancer-specific mortality (PCSM).
Patients and Methods
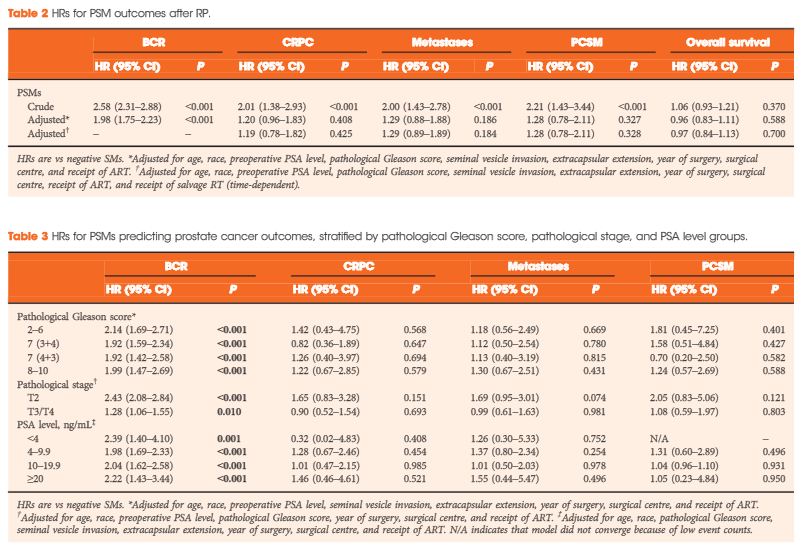
Retrospective study of 4 051 men in the Shared Equal Access Regional Cancer Hospital (SEARCH) cohort treated by RP from 1988 to 2013. Proportional hazard models were used to estimate hazard ratios (HRs) of PSMs in predicting biochemical recurrence (BCR), CRPC, metastases, and PCSM. To determine if PSMs were more predictive in certain patients, analyses were stratified by pathological Gleason score, stage, and preoperative prostate-specific antigen (PSA) level.
Results
The median (interquartile range) follow-up was 6.6 (3.2–10.6) years and 1 127 patients had >10 years of follow-up. During this time, 302 (32%) men had BCR, 112 (3%) developed CRPC, 144 (4%) developed metastases, and 83 (2%) died from prostate cancer. There were 1 600 (40%) men with PSMs. In unadjusted models, PSMs were significantly associated with all adverse outcomes: BCR, CRPC, metastases and PCSM (all P ≤ 0.001). After adjusting for demographic and pathological characteristics, PSMs were associated with increased risk of only BCR (HR 1.98, P < 0.001), and not CRPC, metastases, or PCSM (HR ≤1.29, P > 0.18). Similar results were seen when stratified by pathological Gleason score, stage, or PSA level, and when patients who underwent adjuvant radiotherapy were excluded.
Conclusions
PSMs after RP are not an independent risk factor for CRPC, metastasis, or PCSM overall or within any subset. In the absence of other high-risk features, PSMs alone may not be an indication for adjuvant radiotherapy.