Video: PSMs in RP patients do not predict long-term oncological outcomes
Positive Surgical Margins in Radical Prostatectomy Patients Do Not Predict Long-term Oncological Outcomes: Results from SEARCH
Objective
To assess the impact of positive surgical margins (PSMs) on long-term outcomes after radical prostatectomy (RP), including metastasis, castrate-resistant prostate cancer (CRPC), and prostate cancer-specific mortality (PCSM).
Patients and Methods
Retrospective study of 4 051 men in the Shared Equal Access Regional Cancer Hospital (SEARCH) cohort treated by RP from 1988 to 2013. Proportional hazard models were used to estimate hazard ratios (HRs) of PSMs in predicting biochemical recurrence (BCR), CRPC, metastases, and PCSM. To determine if PSMs were more predictive in certain patients, analyses were stratified by pathological Gleason score, stage, and preoperative prostate-specific antigen (PSA) level.
Results
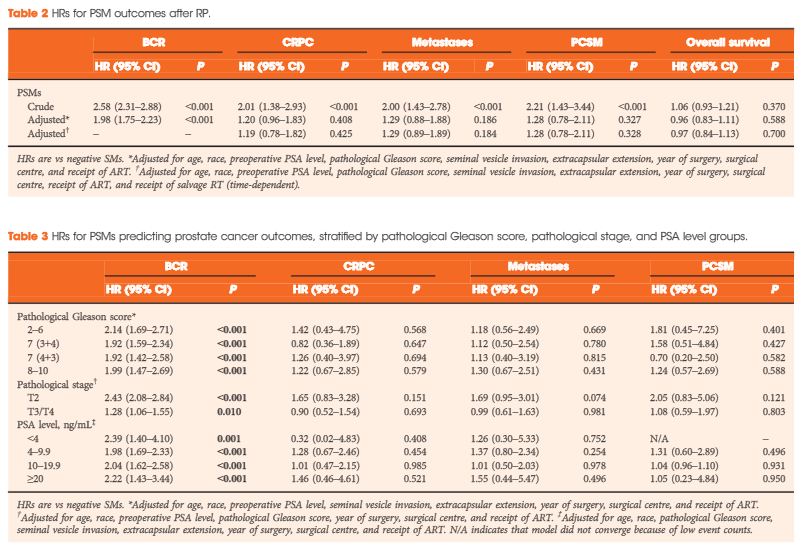
The median (interquartile range) follow-up was 6.6 (3.2–10.6) years and 1 127 patients had >10 years of follow-up. During this time, 302 (32%) men had BCR, 112 (3%) developed CRPC, 144 (4%) developed metastases, and 83 (2%) died from prostate cancer. There were 1 600 (40%) men with PSMs. In unadjusted models, PSMs were significantly associated with all adverse outcomes: BCR, CRPC, metastases and PCSM (all P ≤ 0.001). After adjusting for demographic and pathological characteristics, PSMs were associated with increased risk of only BCR (HR 1.98, P < 0.001), and not CRPC, metastases, or PCSM (HR ≤1.29, P > 0.18). Similar results were seen when stratified by pathological Gleason score, stage, or PSA level, and when patients who underwent adjuvant radiotherapy were excluded.
Conclusions
PSMs after RP are not an independent risk factor for CRPC, metastasis, or PCSM overall or within any subset. In the absence of other high-risk features, PSMs alone may not be an indication for adjuvant radiotherapy.