Article of the week: Remote ischaemic preconditioning reduces injury during partial nephrectomy
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
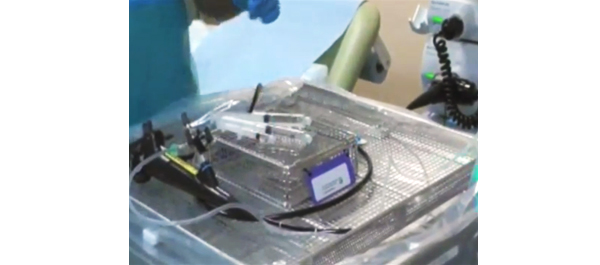
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video by Dr. Huang and colleagues to accompany their article.
If you only have time to read one article this week, it should be this one.
Effect of remote ischaemic preconditioning on renal protection in patients undergoing laparoscopic partial nephrectomy: a ‘blinded’ randomised controlled trial
Jiwei Huang, YongHui Chen, Baijun Dong, Wen Kong, Jin Zhang, Wei Xue, DongMing Liu and Yiran Huang
Department of Urology, Renji Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
OBJECTIVE
• To evaluate whether remote ischaemic preconditioning (RIPC) reduces renal injury in patients undergoing laparoscopic partial nephrectomy (LPN).
PATIENTS AND METHODS
• In all, 82 patients undergoing LPN were randomly assigned to either the RIPC or control group, with 40 and 38 patients, respectively completing 6-months follow-up.
• RIPC was conducted after induction of anaesthesia, which consisted of three 5-min cycles of right lower limb ischaemia and 5 min of reperfusion during each cycle.
• The primary outcome was the absolute change in glomerular filtration rate (GFR) of the affected kidney by renal scintigraphy from baseline to 6 months.
• The secondary outcomes included urinary retinol-binding protein (RBP) levels measured at 24 and 48 h, serum creatinine, and estimated GFR (eGFR) at 1 and 6 months, and changes in GFR by renal scintigraphy.
RESULTS
• There were no differences in the change of GFR of the affected kidney at 6 months, while it was significantly decreased by 15.0% in the control group vs 8.8% in the RIPC group at 1 month (P = 0.034).
• The urinary RBP levels increased 8.4-fold at 24 h in the control group compared with a lower increase of 3.9-fold in the RIPC group (P < 0.001).
• There were no differences in the serum creatinine level or eGFR at 1 and 6 months between the two groups.
CONCLUSIONS
• In patients undergoing LPN, RIPC using transient lower limb ischaemia may reduce renal impairment in the short term, but failed in the longer term despite a non-significant trend in favour of RIPC.
• These novel data support the need for a larger study of RIPC during LPN surgery.
Read Previous Articles of the Week