How our lives have changed. Over two months ago we published a popular blog on the effect of COVID-19 on our surgical practice (https://www.bjuinternational.com/bjui-blog/covid-19-and-urology/). In many ways it informed us as to what to do during challenging times to keep our patients safe.
As we gradually take careful steps out of lockdown, our minds are focused on the most important of all words – SAFETY.
While every nation will have differences and nuances, the principles of learning from each other, remain the same as they did when lockdowns started.
I am not surprised by new and ever changing information about the disease almost every day and see international collaboration as a powerful and positive tool in this situation.
With this in mind I requested our friends from Italy, China, Germany and New Zealand for their own perspectives.
Here are their thoughts for your reading pleasure.
Please feel free to insert your comments under the blog and share on social media.
Yours in friendship,
Prokar Dasgupta
Editor in Chief, BJUI
I am grateful to BJU International for having had the opportunity, around 2 months ago, to share my perspective on the impact of the COVID-19 pandemic on urological practice at Careggi University Hospital in Florence, Italy. I hope that information, coming from an Italian Centre that had to timely re-organize its logistics and surgical schedule in light of the rapid spread of the epidemic across the Country, might have provided some insights for urologists in the UK and worldwide to adapt their own activity during the acute phase of the COVID-19 outbreak.
Herein I am honored to share with you my perspective on how we may safely come out of lockdown, and on what we may learn as a Community from the COVID-19 pandemic to optimize the future organization of urological services.
First of all, I entirely endorse Prof. Dasgupta’s view that, while the way Urology Centres around the world are coping with the challenges raised by the COVID-19 pandemic, as well as the way they are trying to rebuild new “standards” during the “second phase” of the emergency, will certainly vary within Countries, Regions and Hospitals, we as urologists should be open-minded and strive to share and learn as much as possible from each other. As such, in the highly complex scenario we are all living in, every perspective and viewpoint should be leveraged to set new tiles in the “mosaic” of evidence on Urology practice in the post-COVID era.
The status of the COVID-19 epidemic in Italy has significantly changed through the last two months. As of 15th March 2020, the number of laboratory-confirmed cases in Italy was 24 747, with 1809 deaths. As of 14th May 2020, these numbers were 223 096 and 31 368, respectively (making Italy the fifth Country in the world with the higher number of infections, https://lab24.ilsole24ore.com/coronavirus/).
Fortunately, the measures undertaken by the Italian Government so far, including the lockdown, have led to a drastic reduction in the number of daily infections and deaths due to COVID-19, with a progressive parallel decrease in the burden of severely ill patients admitted in ICUs.
However, there is no doubt that this unprecedented pandemic has had a dramatic impact on Italy from all possible standpoints, including the healthcare system. In particular, urology practice has been truly revolutionized during the past two months. Indeed, not only virtually all Centres worldwide have been forced to follow strict schemes for the triage of urological procedures that should have been prioritized in light of the scarcity of resources [1-3], but also Urology training programs have suffered a significant slowdown with potential meaningful consequences on residents’ learning curve [4,5]. As such, while we are now facing the new challenge of dealing with the “adaptation” and forthcoming “chronic” phases of the pandemic (during which all urological services will be progressively reopened to patients) we should keep the focus on preventing nosocomial infection and on cost-effective use of available resources.
In this scenario, the Department of Urology of Careggi University Hospital, directed by Prof. Carini and Prof. Serni, located in Tuscany – one of the five Italian Regions that have been hit most by COVID-19 – has already planned a series of measures aiming to safely restart all Urology services in the coming weeks, ensuring patients and healthcare workers’ safety.
- First, since late March, all patients scheduled for urological procedures (as well as patients undergoing minor surgeries in the outpatient setting, ESWL and prostatic biopsies) had to be tested for Sars-CoV-2 infection (through nasopharyngeal swaps) 48 hours before surgery. Patients who resulted positive for COVID-19 were recommended to remain in quarantine until two consecutive nasopharyngeal swaps resulted negative for the infection. Then, they could have been rescheduled for surgery. In addition, starting from May 1st 2020, all patients undergoing surgery were tested for Sars-CoV-2 infection through nasopharyngeal swaps 24-48 hours before discharge from the Hospital. Of note, patients’ relatives were not allowed to enter the Department during the whole hospitalization period; as such, the news regarding both the intervention and the postoperative course were communicated by the urologists in charge of the inpatient ward by telephone.
- Second, beyond appropriate use of all PPE, all healthcare workers in our Department, including nurses, doctors and administrative staff, underwent serology testing (IgM, IgG) for Sars-CoV-2 infection during the first weeks of April. Those who resulted positive according to the serology underwent further testing with two consecutive nasopharyngeal swaps; if positive, they were recommended to remain in quarantine until two consecutive nasopharyngeal swaps resulted negative for the infection.
- Regarding the Urology operating rooms, we are currently using 50% of them (two out of four) in the main Hospital pavilion, prioritizing major uro-oncological surgery (open and minimally-invasive procedures for prostate, urothelial, and kidney cancer), as well as surgery for penile and testicular cancer. Most endoscopic surgeries for bladder cancer (TURBs) were redeployed in a different Hospital pavilion (in one dedicated operating theater, active four days a week). Overall, the surgical activity of our Urology Department is currently reduced by 20-25% as compared to a “standard” period. Fortunately, we are not facing major concerns regarding the availability of ICU beds for urological patients at our Hospital.
While in the very first weeks after the spread of the epidemic, only high-priority major uro-oncological surgeries (i.e. radical cystectomy, radical prostatectomy for locally-advanced diseases, nephrectomy for cT2+ cancers, radical nephroureterectomy for high-risk upper tract urothelial carcinoma) were performed – accounting for approximately one third of all major cancer surgeries at our Centre based on a recently published study by our group [6]) – later on we progressively included in the surgical schedule also lower-priority interventions (i.e. radical prostatectomy for intermediate-risk prostate cancer, radical/partial nephrectomy for cT1b tumors, etc.).
- Similarly, we progressively reintroduced into the surgical schedules also elective interventions for benign urologic conditions, prioritizing those patients who were symptomatic and/or at higher risk of adverse clinical outcomes. It is important to highlight that the management of the surgical waiting list during the acute phase of the COVID-19 pandemic and the planning of the weekly surgical schedule was performed according to a careful day-by-day evaluation of the available resources in the Hospitals’ ICUs, as well as the number of available theaters for urological procedures.
- Importantly, we did not record any case of COVID-19 after elective or urgent urological procedure during the past two months (including after minimally-invasive surgery, the safety of which has been object of great debate within the Urology Community [7]).
- Regarding urological emergencies, patients who were admitted to our Urology Unit from the Accident & Emergency Department had to be tested for Sars-CoV-2 infection (through nasopharyngeal swaps) before admission. If needed, surgery for urological emergencies was performed in a dedicated operating theater in the main Urology pavilion.
- The kidney transplantation program from deceased donors (both donors after brain death [DBD] and donors after circulatory death [DCD]) continued without major changes at our Unit, thanks to a timely and effective reorganization of all activites related to organ procurement by the Tuscany Transplant Authority, as well as a series of logistical and clinical measures implemented early after the spread of the epidemic to prevent transmission of the disease to KT recipients. On the contrary, kidney transplantation from living donors was (and is still) suspended since the end of February 2020.
- Most urological procedures in the outpatient setting (ESWL, minor surgeries, prostatic biopsies) were canceled during the first weeks of the COVID-19 epidemic, being the only exception cystoscopies for suspected bladder cancer. Thereafter, they were progressively re-started (especially during the last 2 weeks), provided that patients had been tested negative for Sars-CoV-2 infection and anyway after a comprehensive triage by telephone outlining the priority of such procedure.
- Finally, while during the “acute phase” of the pandemic the vast majority of urological consultations in the outpatient setting were canceled (and replaced by telemedicine strategies, except for those visits deemed urgent by urological staff after a careful screening by telephone interview and those for medications after elective surgery). In the coming weeks most of them will be re-started, provided adequate logistics (i.e. distancing between patients and appropriate time schedules) to ensure maximal safety for both patients and healthcare workers.
Overall, the “big picture” delineated by all these facts and figures highlights that our Unit, as in many other Departments in Italy, has already started the process of rebuilding the foundations of a new “routine” urological practice, adapting (and eventually overcoming) to the challenges met during the first acute phase of the COVID-19 emergency.
Nonetheless, my global perspective is that urologists should remain vigilant and resilient, keeping the focus on ensuring safety and cost-effective use of resources. This is important, as the COVID-19 epidemic could potentially flare-up in the near future if all safety measures recommended by Hospitals and the Government were not strictly followed by the population.
Moreover, I believe this unprecedented emergency scenario, which has profoundly revolutionized our healthcare system as well as our way of thinking and behaving, should be leveraged to understand which steps should be prioritized to move Urology forward from both clinical, logistical, educational and scientific perspectives.
In this view, the lessons we can learn as a Community from this pandemic for the future include:
– the need for appropriate (evidence-based) selection of candidates for urological procedures, taking into account also patients’ values and expectations;
– careful prioritization of surgeries, based on the potential impact of delay on important patient outcomes [8];
– rational use of all available treatment modalities for urological cancers (including active surveillance), strengthening the value of team-work and developing a truly multidisciplinary spirit;
– refinement of surgical informed consents, tailoring them to such emergency scenarios [9];
– increased use of virtual Urology learning programs for education of residents [10];
– implementation of teleproctoring and telementoring technologies into everyday surgical practice [11];
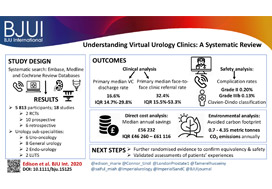
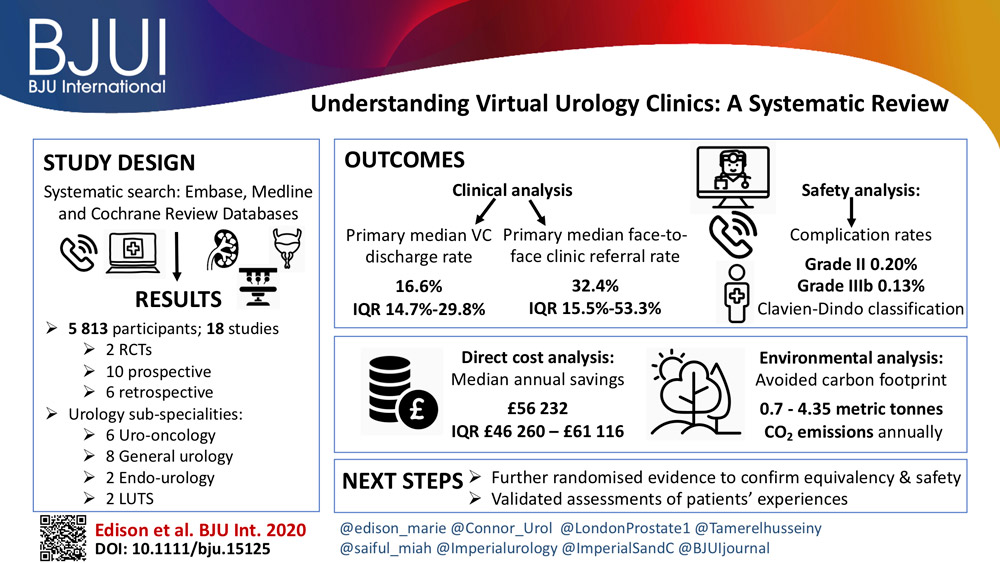
– inclusion of telemedicine into routine pathways of care for urological patients [11].
By doing so, we may be able not only to be more prepared for similar future emergency scenarios, but also to take significant steps toward improvement of Urology as a specialty, as well as ourselves as individuals.
 Riccardo Campi, MD
Riccardo Campi, MD
– Resident in Urology, Dept. of Urology, Careggi University Hospital, Florence (Italy)
– Ph.D. student, Doctoral Program in Clinical Sciences, Dept. of Experimental and Clinical Medicine, University of Florence, Florence (Italy)
– Member of the EAU Young Academic Urologists – Renal Cancer Working Group
– Associate Member of the EAU Section of Oncological Urology
– Twitter: @Ric_Campi
References
[1] Stensland KD, et al. Considerations in the Triage of Urologic Surgeries During the COVID-19 Pandemic. Eur Urol. 2020 doi: 10.1016/j.eururo.2020.03.027.
[2] Ribal MJ, et al. EAU Guidelines Office Rapid Reaction Group: An organisation-wide collaborative effort to adapt the EAU guidelines recommendations to the COVID-19 era. Eur Urol 2020 (In Press); available at: https://www.europeanurology.com/covid-19-resourceEAU
[3] Ahmed K, et al. Global challenges to urology practice during COVID‐19 pandemic. BJU Int 2020. In Press. https://doi.org/10.1111/bju.15082
[4] Amparore D, et al. Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urol Nefrol. 2020. doi: 10.23736/S0393-2249.20.03868-0
[5] Porpiglia F, et al. Slowdown of urology residents’ learning curve during the COVID-19 emergency. BJU Int. 2020 [Epub ahead of print] doi: https://doi.org/10.1111/bju.15076.
[6] Campi R, et al. Assessing the Burden of Nondeferrable Major Uro-oncologic Surgery to Guide Prioritisation Strategies During the COVID-19 Pandemic: Insights from Three Italian High-volume Referral Centres. Eur Urol. 2020 [Epub ahead of print] doi:10.1016/j.eururo.2020.03.054
[7] Novara G, et al. Risk of SARS-CoV-2 Diffusion when Performing Minimally Invasive Surgery During the COVID-19 Pandemic. Eur Urol Apr 2020;0(0). Available at: https://www.europeanurology.com/article/S0302-2838(20)30247-5/abstract
[8] Wallis CJD, et al. Risks from Deferring Treatment for Genitourinary Cancers: A Collaborative Review to Aid Triage and Management During the COVID-19 Pandemic. Eur Urol 2020. In Press. DOI: https://doi.org/10.1016/j.eururo.2020.04.063
[9] Bryan AF, et al. Unknown unknowns: Surgical consent during the COVID-19 pandemic. Annals of Surgery 2020. In Press. https://journals.lww.com/annalsofsurgery/Documents/Unknown%20unknowns%20.pdf
[10] Claps F, et al. Smart Learning for Urology Residents during the COVID-19 pandemic and beyond: Insights from a Nationwide Survey in Italy. Minerva Urol Nefrol 2020. In Press.
[11] Karim JS, et al. Bolstering the surgical response to COVID‐19: how virtual technology will save lives and safeguard surgical practice. BJU Int 2020. In Press. https://doi.org/10.1111/bju.15080
[12] Connor MJ, et al. COVID‐19 pandemic – is virtual urology clinic the answer to keeping the cancer pathway moving? BJU Int 2020. In Press. https://doi.org/10.1111/bju.15061