Posts
Video: Resident burnout in USA and European urology residents
Resident burnout in USA and European urology residents: an international concern
Abstract
Objective
To describe the prevalence and predictors of burnout in USA and European urology residents, as although the rate of burnout in urologists is high and associated with severe negative sequelae, the extent and predictors of burnout in urology trainees remains poorly understood.
Subjects and methods
An anonymous 32‐question survey of urology trainees across the USA and four European countries, analysing personal, programme, and institutional factors, was conducted. Burnout was assessed using the validated abridged Maslach Burnout Inventory. Univariate analysis and multivariable logistic regression models assessed drivers of burnout in the two cohorts.
Results
Overall, 40% of participants met the criteria for burnout as follows: Portugal (68%), Italy (49%), USA (38%), Belgium (36%), and France (26%). Response rates were: USA, 20.9%; Italy, 45.2%; Portugal, 30.5%; France, 12.5%; and Belgium, 9.4%. Burnout was not associated with gender or level of training. In both cohorts, work–life balance (WLB) dissatisfaction was associated with increased burnout (odds ratio [OR] 4.5, P < 0.001), whilst non‐medical reading (OR 0.6, P = 0.001) and structured mentorship (OR 0.4, P = 0.002) were associated with decreased burnout risk. Lack of access to mental health services was associated with burnout in the USA only (OR 3.5, P = 0.006), whilst more weekends on‐call was associated with burnout in Europe only (OR 8.3, P = 0.033). In both cohorts, burned out residents were more likely to not choose a career in urology again (USA 54% vs 19%, P < 0.001; Europe 43% vs 25%, P = 0.047).
Conclusion
In this study of USA and European urology residents, we found high rates of burnout on both continents. Despite regional differences in the predictors of burnout, awareness of the unique institutional drivers may help inform directions of future interventions.
July 2019 – About the cover

The Article of the Month for July is the latest NICE guideline on prostate cancer – diagnosis and management. The National Institute for Health and Care Excellence (NICE) based in London, UK was established in 1999 to provide national guidance and advice to improve health and social care. It has published over 50 documents covering urology, including guidance, advice and pathways. Since 2012 NICE has also been responsible for social care guidance. Although its main focus is England, NICE has gained an international reputation as a role model for developing clinical guidelines and providing assessments of new technologies.
The cover image shows the UK from space with the northern lights over the horizon. The best place in the UK to see the northern lights is in the northern part of Scotland, however, if the conditions are right they can be seen as far south as Cornwall.
© istock.com/Elen11
What’s the diagnosis?
Why attend Advanced Prostate Cancer Consensus Conference APCCC 2019?
From the 29th to the 31st of August 2019 the next Advanced Prostate Cancer Consensus Conference #APCCC19 will take place in Basel, Switzerland. The consensus conference was inspired by the very successful and pioneering early breast cancer consensus conference that was started in 1978 in St Gallen.
APCCC was initiated in 2015 because of the rapid developments in the field of advanced prostate cancer with the aim to discuss the clinical management of men with advanced prostate cancer, with a special focus on situations with a lack of or only weak evidence from the literature or conflicting evidence. Prostate cancer is such a common disease that the majority of men across the globe are not treated in expert centers but rather in smaller hospitals or community-based practices. APCCC wants to help the process of knowledge translation by assembling a large group of international prostate cancer experts that hold highly educational lectures summarizing the available literature and evidence, and discussing controversial questions.
The recommendations from the previous two conferences in 2015 and 2017 have been published open access in renowned scientific journals and have been widely read:

The expert panel in action at APCCC 2017
The following topics have been chosen for discussion at the 2019 conference:
- Locally advanced prostate cancer
- Biochemical recurrence of prostate cancer after local therapy
- Management of primary tumour in the metastatic situation
- Newly diagnosed metastatic prostate cancer, including oligometastatic prostate cancer
- Management of nmCRPC
- Management of mCRPC
- Bone and bone metastases
- Molecular characterization: tissue and blood
- Heterogeneity of men with prostate cancer (ethnicity, elderly)
- Side effects of hormonal treatments and their management

Difficult questions at APCCC17
Importantly all participants of APCCC can attend the consensus discussion and voting on Saturday morning. The questions and voting results will again form the basis for a report that will be published soon after the conference.
Why attend APCCC 2019?
The management of men with advanced prostate cancer keeps changing rapidly. Practice changing results have been recently presented and controversially discussed at ESMO (e.g. radiation therapy of the primary in the metastatic situation) and important new data will be presented at ASCO 2019 (e.g. results of standard-of-care therapy with or without enzalutamide or apalutamide for metastatic hormone-sensitive prostate cancer), making the choice of treatment in this situation even more challenging.
There are many reasons to attend APCCC 2019:
- A unique opportunity to focus on the important topic of advanced prostate cancer management for two and a half days and be updated on current standards and state of the art of the care of men with advanced prostate cancer
- Be involved in a global discussion on questions relevant to daily clinical practice but not investigated well

Expert interactions at APCCC17
- Help to translate the outcomes from clinical trials into the management of men with prostate cancer in daily practice especially for men treated outside of large prostate cancer centers.
- Be inspired and organize an APCCC satellite meeting for your country or region as has been done after the previous consensus conferences, with manuscripts published here in the BJUI.
- Chiong et al. The Asia-Pacific Satellite of the APCCC BJUI 2019
- Ma WK et al. Consensus statements on the management of clinically localized prostate cancer from the Hong Kong Urological Association and the Hong Kong Society of Uro-Oncology BJU Int. 2019
- Omlin A, Gillessen S. The Advanced Prostate Cancer Consensus on a regional level – what can we learn? BJU Int. 2019
- And of course, enjoy a few wonderful summer days in the beautiful city of Basel!!!
Further information and links
Preview of APCCC 2019: Silke Gillessen, in conversation with Alicia Morgans, discusses many of the changes we have experienced in clinical practice since the last APCCC in 2017
APCCC on the THE “NEW” PROSTATE CANCER INFOLINK
by Dr Aurelius Omlin
Twitter: @apccc19
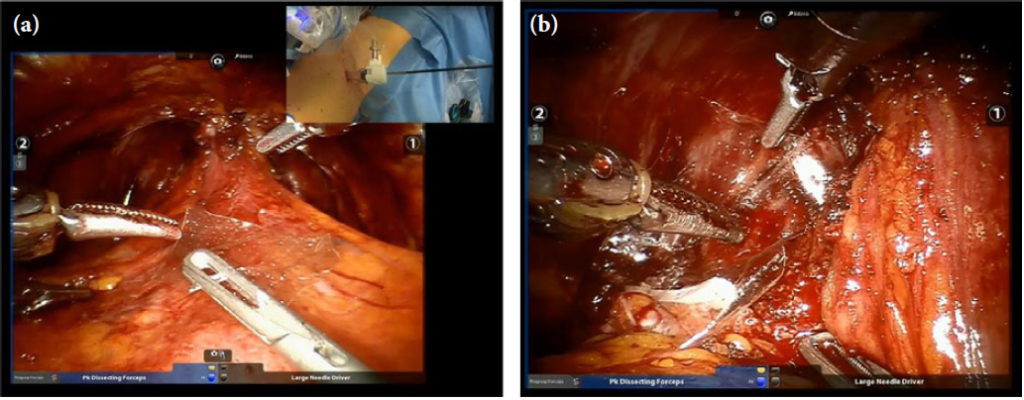
Video: Prostatic capsular incision during RP has important oncological implications. A systematic review and meta‐analysis
Prostatic capsular incision during radical prostatectomy has important oncological implications. A systematic review and meta‐analysis
Abstract
Introduction
Capsular Incision (CapI) is an iatrogenic breach of the prostatic capsule during radical prostatectomy that can cause positive surgical margins (PSM) in organ‐confined (pT2) prostate cancer (PCa), or the retention of benign prostatic tissue. We systematically interrogated the literature in order to clarify the definition of CapI, and the implications of this event for rates of PSM and biochemical recurrence (BCR).
Methods
A literature search was conducted according to PRISMA criteria using the search terms ‘CapI’ AND ‘prostatectomy’ and variations of each. 18 studies were eligible for inclusion.
Results
A total of 51,057 radical prostatectomy specimens were included. The incidence of CapI ranged from 1.3‐54.3%. CapI definitions varied, and included a breach of the prostatic capsule “exposing both benign or malignant PCa cells”, “malignant tissue only”, or “benign tissue only”. The incidence of PSM due to CapI ranged from 2.8 – 71.7%. Our meta‐analysis results found that when CapI was defined as “exposing malignant tissue only in organ‐confined prostate cancer” there was an increased risk of BCR compared to patients with pT2 disease and no CapI (RR 3.53, 95%CI 2.82‐4.41; p < 0.00001).
Conclusions
The absolute impact of CapI on oncological outcomes is currently unclear due to inconsistent definitions. However, the data implies an association between CapI and PSM and BCR. Reporting of possible areas of CapI on the operation note, or marking areas of concern on the specimen, are critical to assist CapI recognition by the pathologist.
What’s the diagnosis?
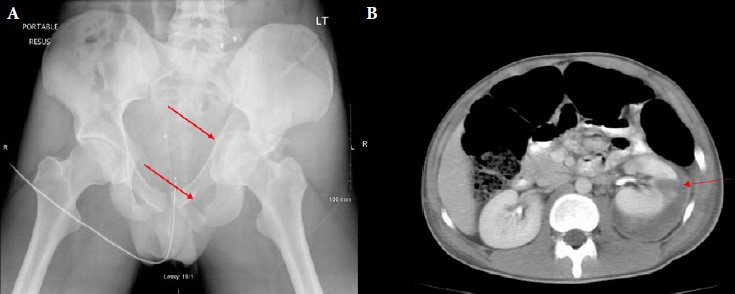
These images are part of a series from Bhatt et al, BJUI 2018 showing concomitant genitourinary injuries and pelvic/ acetabular trauma.
No such quiz/survey/poll
What’s the diagnosis?
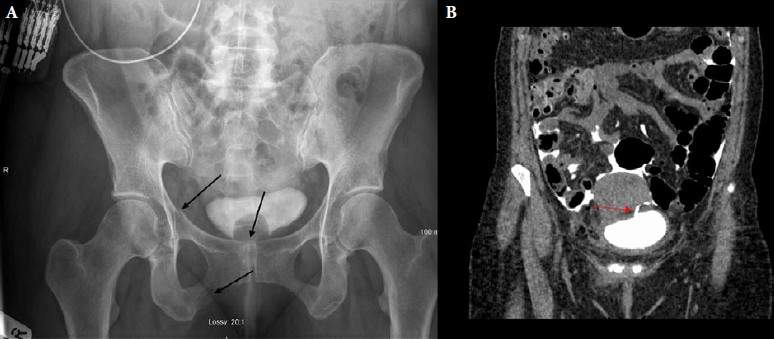
These images are part of a series from Bhatt et al, BJUI 2018 showing concomitant genitourinary injuries and pelvic/ acetabular trauma.
No such quiz/survey/poll