EAU19 Barcelona – Highlights from days 3-5 of the 34th Annual EAU Congress
The early Sunday morning start did not deter delegates from attending one of the three packed plenary sessions of the day. They covered a broad range of rapidly changing areas in urology from imaging in prostate cancer, an update on renal cell carcinoma (RCC) and the breaking news session discussing the potentially game changing results from the recent ARAMIS study and new research into fast bi-parametric MRI. The role of imaging in prostate cancer is swiftly evolving, with the plenary discussion focusing on recent changes in the diagnostic pathway of localised prostate cancer, particularly with the use of MRI. Next door in the RCC plenary, the speakers debated ‘knife, needle or nothing?’ for the small renal mass in the young patient followed by an update on the very recent and potentially guideline-changing advances in systemic therapy for RCC.
The mid-morning thematic sessions covered the full spectrum of urology from semi-live surgery, the newest advances in immunotherapy, imaging and even how to run a urology office in Europe.
The 7th BJUI social media awards on Sunday night were again the social highlight of the EAU. A view of the Museu Nacional d’Art de Catalunya provided a stunning backdrop to the packed event, with the stars of #UroSoMe recognised for their outstanding work. The night kicked off with the award for the most read blog going to social media champion Professor Declan Murphy.
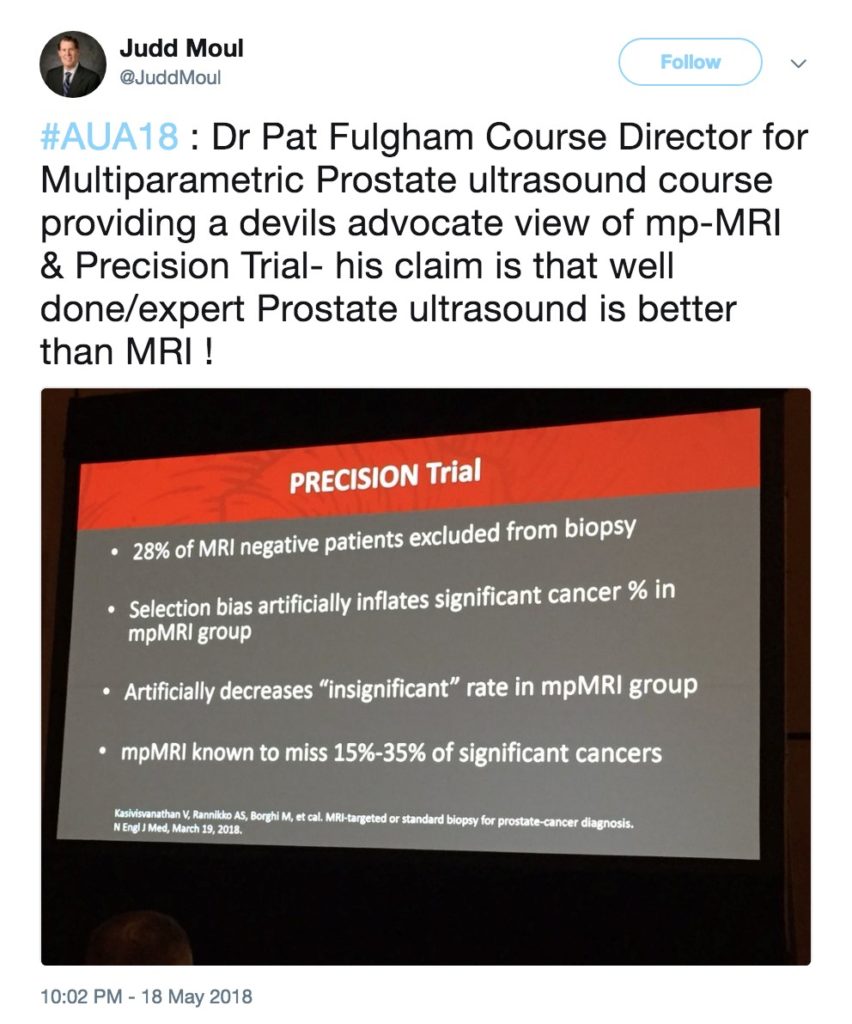
#EAU19 @BJUIjournal #UroSoMe Awards: Most read blog goes to @declangmurphy himself re: Precision Trial @veerukasi @mrsprostate pic.twitter.com/zz2r8LxM0Z
— Abdullatif Aydın (@abdullatif_aydn) March 17, 2019
The awards highlighted the far reaching and valuable impact of social media, recognising a number of important achievements in the field such as Nature Reviews Urology for ‘Both sides of the scalpel: the patient and surgeon view’ with a special guest video appearance from Stephen Fry.
Massive thanks @BJUIjournal for the award for @benchallacombe & @stephenfry's article. Huge surprise &the special video from Stephen was amazing 😭. It's been an honour& I'm so proud to have produced something that has had such a positive impact. That's it; I've peaked. #eau19 pic.twitter.com/7cb6NEiqYY
— Nette Fenner is in the shed (@NetteFenner) March 18, 2019
However, for me the most special part of the night was seeing my friend Daniel Christidis remembered and honoured with the most ‘social’ trainee award. Dan was a leader in the real and #UroSoMe world (and had personally set up my Twitter account, and those of many of the other young attendees that night) and I know would have been proud to be remembered for one of the things he did so well.
Honoured to collect this award on behalf of amazing trainee and friend @dan_christidis 🌟 loved and missed all around the world @DocToddManning @dr__shanza @AusYURO Thank you @declangmurphy @prokarurol @MattBultitude @BJUIjournal #UroSoMe #EAU19 #rooftopparty https://t.co/AcUtx7Rf2G
— Sophie R-H (@urologytrainee) March 17, 2019
After the BJUI social media awards, it was time for a little black-tie glamour with the EAU19 Friendship Dinner at the historical Casa Llotja de Mar. The night started with a welcome from Professor Christopher Chapple underlining the importance of international partnerships in urology, followed by a fantastic night of good food, wine and enjoying the beautiful Catalan Gothic architecture.
Professor Chris Chapple, Secretary General of the EAU, highlights international collaboration in urology at the friendship dinner. #EAU19 pic.twitter.com/0WrbUsBkcm
— Kathleen Kobashi (@KKseattle) March 18, 2019
The Monday morning plenary sessions delivered another jam-packed morning of a mix of cutting-edge science, quality of life issues in cancer survivorship and prostate cancer. The breaking news session discussed the primary results from SAUL, confirming tolerability and safety of atezolizumab in real-world mUC patients, and the results of ARCHES, which investigated the efficacy of androgen deprivation therapy with enzalutamide or placebo in metastatic hormone-sensitive prostate cancer. The controversies in prostate cancer were again debated in an interactive and diverse way between ‘jury members’ including a geriatrician, psychologist, radiation oncologist and urologist.
The last day of the thematic sessions of the congress again provided a smorgasbord of topics in urology. Later in the day, the expert-guided poster tours gave delegates a chance to navigate the huge number of posters from guidelines to local treatment of prostate cancer.
The closing plenary on Tuesday morning to a full auditorium gave a sweeping overview of the top contributions to EAU19 leaving us with a free half day to explore our generous host city and take in the stunning architecture, food and sunshine!


Bustling Barcelona provided the perfect backdrop to a well organised, action packed conference which featured world leading urologists and scientists from around the world presenting practice changing new data. Cannot wait for EAU 2020 in Amsterdam! #EAU20 #Amsterdam #UroSoMe
by Jiasian Teh, Urology Registrar, PhD Candidate, Peter MacCallum Cancer Centre