March 2017 #urojc summary: Pelvic Lymph Node Dissection with Radical Prostatectomy – Is there enough evidence for and against?
The twitter-based international urology journal club @iurojc #urojc is back with a splash after a brief hiatus. For the March 2017 #urojc, a lively discussion takes the theme of pelvic node dissection (PLND) on radical prostatectomy (RP) reviewing a timely article by Nicola Fossati et al. The paper was made available open access courtesy of European Urology @EUplatinum.
Benefits and Harms of Different Extents of LND During Radical Prostatectomy for #ProstateCancer: A https://t.co/PxRbbUyQOM
— European Urology (@EUplatinum) February 13, 2017
A systematic review of the literature was performed including all comparative studies of both randomized and non randomized studies, with at least one experimental and one control arm. This summarised 66 studies including more than 250.000 patients with particular focus on different extents of pelvic lymphadenectomy as proposed by the European Association of Urology. Outcome measures studied included oncological features of biochemical recurrence, development of metastases, cancer-specific survival, and overall survival. Adverse events were covered under secondary outcomes, both intra- and postoperatively observed. Finally, quality of PLND was addressed in terms of total number of nodes and total number of positive nodes. Risk of bias was assessed for all studies judging on basis of specific confounders.
The journal club ran for 48 hours from Sunday 5th march. The central question addressed is balance of benefits and drawbacks of lymph node dissection. The corresponding author of the manuscript, Steven Joniau from the University Hospitals of Leuven, Belgium highlighted the role of lymph nodes in prostate cancer recurrence.
#urojc Remember: PCa recurrence often first in regional LN. So, why not remove at RP? @iurojc @ChapinMD @LoebStacy @EveraertsW @dr_coops pic.twitter.com/5GRKhjOJfl
— steven joniau (@joniau) March 6, 2017
However despite this idea, the benefit of PLND is heavily scrutinized from the start. Long term data from a single centre suggested limited benefit.
How do we reconcile what appears to be lack of therapeutic benefit & morbidity for ePLND and current guidelines? #urojc
— Urology JC #urojc (@iurojc) March 5, 2017
Depends on how much time you spend on it😀 JH population was "unique". Therapeutic benefit depends on the cohort being studied.
— Badar M. Mian, MD (@BadarMian1) March 5, 2017
If PSA bcf so high with N1 disease, has PLND really made a diff? How is management changed if N1 disease confirmed pathologically? #urojc
— Urology JC #urojc (@iurojc) March 6, 2017
However PLND has since earlier times been employed as a diagnostic tool, where an optimal template (presacral in addition to extended LND) may be optimal for staging and removal of lymph nodes.
Does need for accurate staging trump (NOT about that man 😊) therapeutic benefit for standard PLND versus ePLND?#urojc pic.twitter.com/6N3bjAoRS2
— Urology JC #urojc (@iurojc) March 5, 2017
Try to encourage in our MDT as node info is often can often fine tune further management after RP #urojc https://t.co/4fZQ2eEVkv
— Nick Brook (@nickbrookMD) March 5, 2017
#urojc But knowlegde gained by PLND may guide decisions regarding adj treatment (which may influence survival)
— steven joniau (@joniau) March 6, 2017
Prospective study shows 'less-than-eLND' insuficient for staging. eLND 94% accurate staging, but misses 24% pos LN compared to seLND pic.twitter.com/f1Fm26SPcp
— steven joniau (@joniau) March 6, 2017
Despite the current state of evidence, PLND is frequently mentioned in the various guidelines available for prostate cancer. However the exact situations when to employ them is questioned by some participants.
How do we reconcile what appears to be lack of therapeutic benefit & morbidity for ePLND and current guidelines? #urojc
— Urology JC #urojc (@iurojc) March 5, 2017
@iurojc @nickbrookMD #EAUGuidelines mention Briganti, MSKCC or Roach nomograms, NCCN doesn't recommend a particular nomogram #urojc pic.twitter.com/QAdE4PBsHa
— Stacy Loeb, MD (@LoebStacy) March 6, 2017
#urojc @joniau @ChapinMD @LoebStacy @dr_coops Makes sense for high risk tumours, but the EAU 5% guideline for PLND is overkill
— Wouter Everaerts (@EveraertsW) March 6, 2017
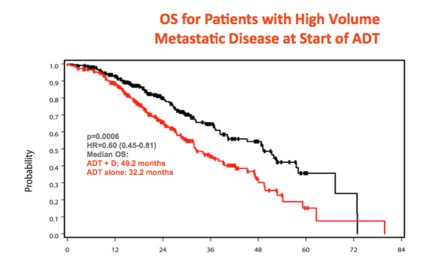
The various therapeutic options for lymph node metastases also coloured the discussion.
if we can figure out whether postop RT necessary in all N1, ePLND may help avoid unnecessary treatment in some. #urojc
— Brian F. Chapin (@ChapinMD) March 6, 2017
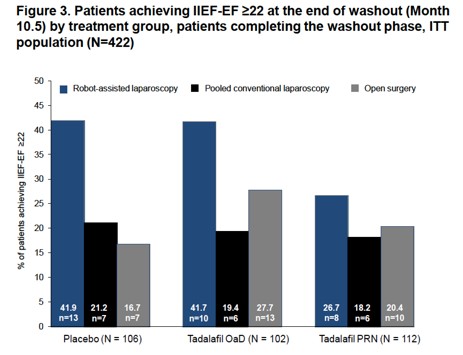
The discussion further continued to the important issue of morbidity, and the associated question of performing an extended PLND (ePLND).
Are we understating morbidity of ePLND? Do we leave these patient on a knifes edge for future lymphodema? (Eg future RT, infection)#urojc
— Urology JC #urojc (@iurojc) March 6, 2017
@joniau lymphoedema is major concern for QoL, especially after eLND+ adj RT,
Needs multiD management #urojc— Wouter Everaerts (@EveraertsW) March 6, 2017
the baby shouldn't be in the bath. PLND so clearly needs to be tested in a prospective trial. As for ePLND…
— Tim O'Brien (@tsoburol) March 6, 2017
What's your justification for doing an ePLND? Is it because of guideline recommendations?#urojc
— Urology JC #urojc (@iurojc) March 5, 2017
#urojc ePLND = mmmPLND, more morbidity,minutes,money. less BCR, doubt it.
— Alan Hay (@alanhaymd) March 5, 2017
@iurojc ePLND does nearly double my time for RALRP. Sometimes even longer then the prostatectomy. #urojc
— Brian F. Chapin (@ChapinMD) March 6, 2017
.@DrHWoo I don't follow–Some N+ men essntlly cured by only RP/PLND. I think it's therapeutic.
But I don't believe ePLND= improvemnt #urojc pic.twitter.com/EwSp4Im5VO— David Y.T. Chen (@dytcmd) March 6, 2017
Try to encourage in our MDT as node info is often can often fine tune further management after RP #urojc https://t.co/4fZQ2eEVkv
— Nick Brook (@nickbrookMD) March 5, 2017
#urojc But knowlegde gained by PLND may guide decisions regarding adj treatment (which may influence survival)
— steven joniau (@joniau) March 6, 2017
Prospective study shows 'less-than-eLND' insuficient for staging. eLND 94% accurate staging, but misses 24% pos LN compared to seLND pic.twitter.com/f1Fm26SPcp
— steven joniau (@joniau) March 6, 2017
Despite the current state of evidence, PLND is frequently mentioned in the various guidelines available for prostate cancer. However the exact situations when to employ them is questioned by some participants.
How do we reconcile what appears to be lack of therapeutic benefit & morbidity for ePLND and current guidelines? #urojc
— Urology JC #urojc (@iurojc) March 5, 2017
@iurojc NCCN guidelines recommend PLND for nomogram probability >=2% vs 5% threshold in #eauguidelines #urojc pic.twitter.com/7HYVSYUSJv
— Stacy Loeb, MD (@LoebStacy) March 6, 2017
@iurojc @nickbrookMD #EAUGuidelines mention Briganti, MSKCC or Roach nomograms, NCCN doesn't recommend a particular nomogram #urojc pic.twitter.com/QAdE4PBsHa
— Stacy Loeb, MD (@LoebStacy) March 6, 2017
#urojc @joniau @ChapinMD @LoebStacy @dr_coops Makes sense for high risk tumours, but the EAU 5% guideline for PLND is overkill
— Wouter Everaerts (@EveraertsW) March 6, 2017
The
if we can figure out whether postop RT necessary in all N1, ePLND may help avoid unnecessary treatment in some. #urojc
— Brian F. Chapin (@ChapinMD) March 6, 2017
The discussion further continued to the important issue of morbidity, and the associated question of performing an extended PLND (ePLND).
Are we understating morbidity of ePLND? Do we leave these patient on a knifes edge for future lymphodema? (Eg future RT, infection)#urojc
— Urology JC #urojc (@iurojc) March 6, 2017
@joniau lymphoedema is major concern for QoL, especially after eLND+ adj RT,
Needs multiD management #urojc— Wouter Everaerts (@EveraertsW) March 6, 2017
the baby shouldn't be in the bath. PLND so clearly needs to be tested in a prospective trial. As for ePLND…
— Tim O'Brien (@tsoburol) March 6, 2017
What's your justification for doing an ePLND? Is it because of guideline recommendations?#urojc
— Urology JC #urojc (@iurojc) March 5, 2017
#urojc ePLND = mmmPLND, more morbidity,minutes,money. less BCR, doubt it.
— Alan Hay (@alanhaymd) March 5, 2017
@iurojc ePLND does nearly double my time for RALRP. Sometimes even longer then the prostatectomy. #urojc
— Brian F. Chapin (@ChapinMD) March 6, 2017
.@DrHWoo I don't follow–Some N+ men essntlly cured by only RP/PLND. I think it's therapeutic.
But I don't believe ePLND= improvemnt #urojc pic.twitter.com/EwSp4Im5VO— David Y.T. Chen (@dytcmd) March 6, 2017
if we can figure out whether postop RT necessary in all N1, ePLND may help avoid unnecessary treatment in some. #urojc
— Brian F. Chapin (@ChapinMD) March 6, 2017
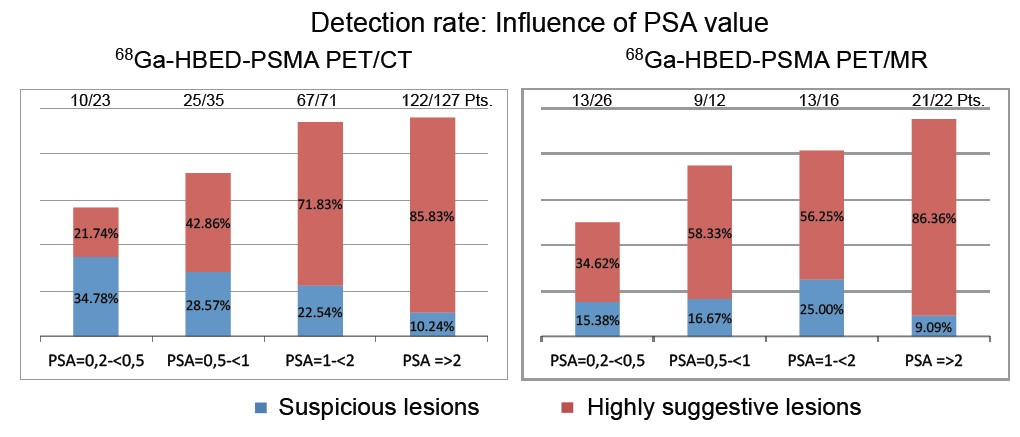
The increasing use of PSMA PET/CT provided other spread pattern data to be considered. And finally temporal changes in PSA testing is observed to affect the need for LND.
How might Ga68 PSMA PET/CT change the dynamic? Early data shows a lot of disease above the diaphragm. #urojc https://t.co/zyX9czHuwH
— Urology JC #urojc (@iurojc) March 6, 2017
Although, with PSMA PET/CT we're finding crazy spread patterns (e.g. Isolated supraclav nodal met) #urojc
— Matt Cooperberg (@dr_coops) March 6, 2017
I dunno… in 2017 I think it's a very rare pt who needs the RP and doesn't need the LND! #urojc @iurojc
— Matt Cooperberg (@dr_coops) March 6, 2017
#urojc @dr_coops @LoebStacy @iurojc the pt who "doesn't need PLND" probably often doesn't need RP either. Especially in PSA era
— David Y.T. Chen (@dytcmd) March 6, 2017
From the poll which ran during the discussion, about half responders would perform extended PLND for staging, while the rest were divided almost equally between therapeutic benefit and adherence to guideline recommendations.
Why do you do ePLND?#urojc
— Urology JC #urojc (@iurojc) March 5, 2017
Probably all participants of the discussion agrees for the need of a proper randomised study addressing role of PLND.
But "therapeutic benefits of PLND during radical prostatectomy remain unproven"@ChapinMD @LoebStacy @EveraertsW @dr_coops#urojc
— Henry Woo (@DrHWoo) March 6, 2017
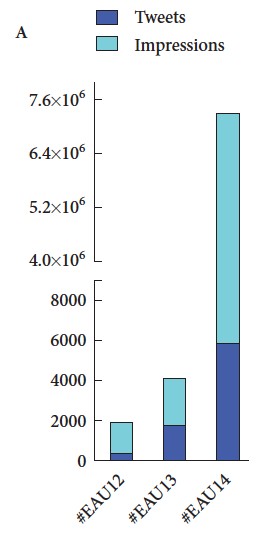
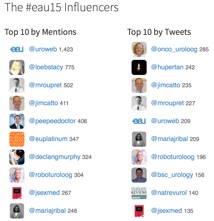
At the end of a busy 48 hours, the discussion had been joined by top experts in the field of prostate cancer, generated more than 200 tweets and reached more than 700 thousand impressions the world over.
Special thanks to @EUplatinum for allowing open access for this month's paper. Special thanks to author @joniau for participating #urojc
— Urology JC #urojc (@iurojc) March 7, 2017
Yodi Soebadi (@yodisoebadi) is an Indonesian urologist, trained at Universitas Airlangga, currently pursuing doctoral research at KU Leuven in Belgium.