Posts
Article of the week: Development of a side‐specific, mpMRI‐based nomogram for the prediction of extracapsular extension of PCa
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there are two accompanying editorials written by prominent members of the urological community. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation. There is also a video produced by the authors.
If you only have time to read one article this week, it should be this one.
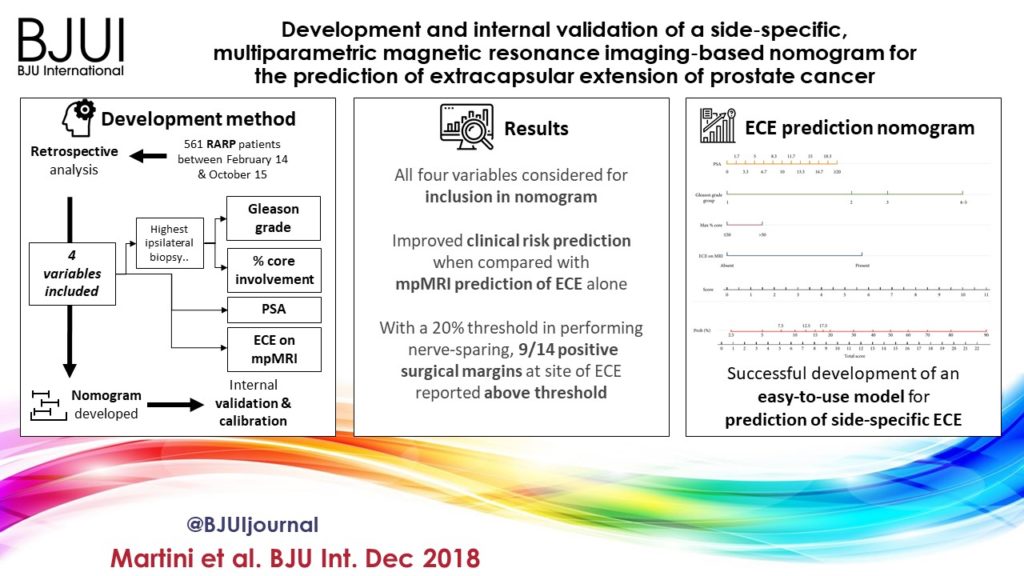
Development and internal validation of a side‐specific, multiparametric magnetic resonance imaging‐based nomogram for the prediction of extracapsular extension of prostate cancer
Abstract
Objectives
To develop a nomogram for predicting side‐specific extracapsular extension (ECE) for planning nerve‐sparing radical prostatectomy.
Materials and Methods
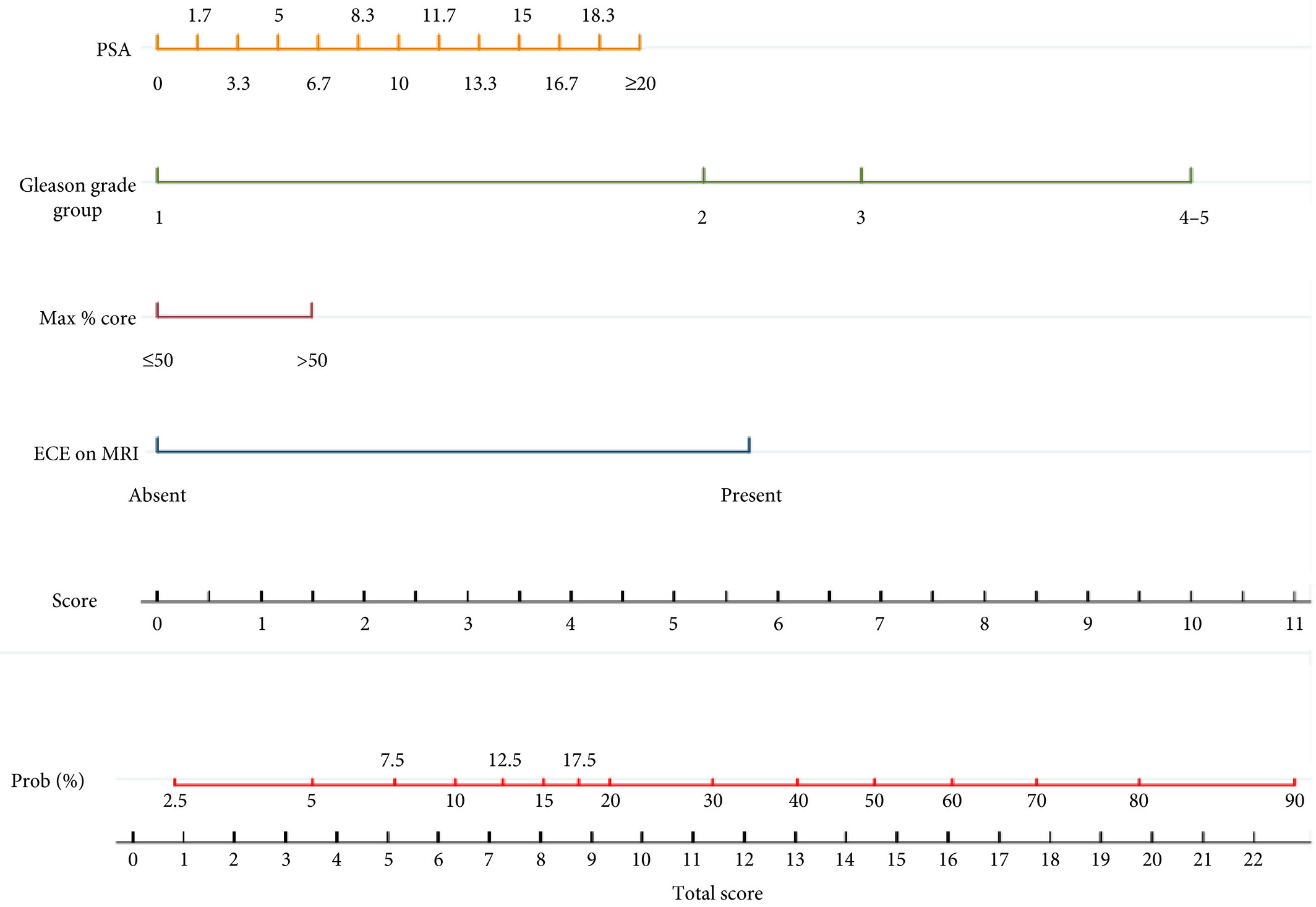
We retrospectively analysed data from 561 patients who underwent robot‐assisted radical prostatectomy between February 2014 and October 2015. To develop a side‐specific predictive model, we considered the prostatic lobes separately. Four variables were included: prostate‐specific antigen; highest ipsilateral biopsy Gleason grade; highest ipsilateral percentage core involvement; and ECE on multiparametric magnetic resonance imaging (mpMRI). A multivariable logistic regression analysis was fitted to predict side‐specific ECE. A nomogram was built based on the coefficients of the logit function. Internal validation was performed using ‘leave‐one‐out’ cross‐validation. Calibration was graphically investigated. The decision curve analysis was used to evaluate the net clinical benefit.
Results
The study population consisted of 829 side‐specific cases, after excluding negative biopsy observations (n = 293). ECE was reported on mpMRI and final pathology in 115 (14%) and 142 (17.1%) cases, respectively. Among these, mpMRI was able to predict ECE correctly in 57 (40.1%) cases. All variables in the model except highest percentage core involvement were predictors of ECE (all P ≤ 0.006). All variables were considered for inclusion in the nomogram. After internal validation, the area under the curve was 82.11%. The model demonstrated excellent calibration and improved clinical risk prediction, especially when compared with relying on mpMRI prediction of ECE alone. When retrospectively applying the nomogram‐derived probability, using a 20% threshold for performing nerve‐sparing, nine out of 14 positive surgical margins (PSMs) at the site of ECE resulted above the threshold.
Conclusion
We developed an easy‐to‐use model for the prediction of side‐specific ECE, and hope it serves as a tool for planning nerve‐sparing radical prostatectomy and in the reduction of PSM in future series.
Editorial: A novel nomogram for predicting ECE of prostate cancer
We read with great interest the publication on the side‐specific multiparametric magnetic resonance imaging (mpMRI)‐based nomogram from Martini et al. [1].
The prediction of extracapsular extension (ECE) of prostate cancer is of utmost importance to inform accurate surgical planning before radical prostatectomy (RP).
Today, surgical strategy is tailored to the patient’s characteristics, and the need for a correct prediction of ECE is of paramount importance to guarantee oncological safety, as well as optimal functional outcome. The most up‐to‐date guidelines suggest referring to nomograms to decide whether or not to perform nerve‐sparing (NS) surgery. Since the first version of the Partin Tables in 1993, several models have been developed based on PSA, Gleason score at prostate biopsy, and clinical staging, as the most used covariates.
Furthermore, mpMRI is increasingly used in the diagnostic pathway of prostate cancer to aid prostate biopsy targeting and to attain a more accurate diagnosis of clinically significant prostate cancer. Despite its recognised role in the detection of cancer, the accuracy for local staging is poor, providing a low and heterogeneous sensitivity for the detection of ECE [2].
Given this limitation, the addition of MRI to clinically derived nomograms might result in an improved assessment of preoperative local staging. In a retrospective analysis of 501 patients who underwent RP, MRI + clinical models outperformed clinical‐based models alone for all staging outcomes, with better discrimination in predicting ECE with MRI + Partin Tables and MRI + Cancer of the Prostate Risk Assessment (CAPRA) score than nomograms alone [3].
In the current article, Martini et al. [1] suggest a novel nomogram for predicting ECE that includes the presence of a ‘documented definite ECE at mpMRI’ as an additional variable beyond PSA, Gleason score, and maximum percentage of tumour in the biopsy core with the highest Gleason score. Readers should recognise that this is the first model integrating side‐specific MRI findings together with side‐specific biopsy data to provide a ‘MRI‐based side‐specific prediction of ECE’, in an effort to support the surgical decision for a uni‐ or bilateral NS approach.
However, given the frail generalisability of nomograms in different datasets even after external validation [4], a predictive tool has to be built on a rigorous methodology with clear reproducibility of all steps the covariates derive from.
In this respect, the current model raises some concerns.
The schedule of preoperative MRI assessment is arbitrary, with imaging being performed either before (23.9%) or after systematic biopsy (76.1%), and amongst patients with a MRI prior to biopsy, only 94 of 134 patients underwent additional targeted sampling. As a result, MRI is applied by chance in three different ways: before prostate biopsy without targeted sampling, before prostate biopsy with targeted sampling, and after prostate biopsy.
Based upon this heterogeneous MRI timing, the performance of such a model in a novel population may be biased depending on the diagnostic pathway applied at each institution.
The choice of the variables included represents another point of concern. The output of two out of four covariates, ECE depiction at mpMRI and the percentage of tumour in the biopsy core, have been deliberately dichotomised, without taking into account the continuous trend intrinsic to both variables.
Actually, local staging in the European Society of Urogenital Radiology (ESUR) guidelines has been scored on a 1–5 point scale to grade the likelihood of an ECE event. The authors deliberately dichotomised mpMRI findings, considering ‘the loss of prostate capsule and its irregularity’ as suggestive of ECE and ‘broad capsular contact, abutment or bulge without gross ECE’ evocative of organ‐confined disease. As a result, the included MRI covariate may account for a gross prediction of ECE, maintaining the inaccurate and inter‐reader subjective interpretation of local staging intrinsic to MRI.
Beyond those methodological concerns and the moderate sample size that may limit the reproducibility of the model, we wonder if such a prediction really assists the surgeon’s capability to perform a tailored surgery.
The ‘all or none’ era of NS surgery is over, and we are currently able to grade NS according to different approaches reported in the literature. Particularly, Tewari et al. [5] proposed a NS approach based on four grades of dissection, with the veins on the lateral aspect as vascular landmarks to gain the correct dissection planes. Patel et al. [6] described a five‐grade scale of dissection, using the arterial periprostatic vasculature as a landmark to the same purpose.
If we are able to grade a NS surgery, the prediction of ECE should be graded as well and should answer the prerequisite of knowing the amount of prostate cancer extent outside the capsule. How does a surgeon make the decision to follow a more or less conservative dissection otherwise?
We tried to address this issue by using a tool aimed at predicting the amount of ECE [the Predicting ExtraCapsular Extension in Prostate cancer tool] [6] and supporting the choice of the correct plane of dissection with a suggested decision rule. In our study, developed on a large sample of nearly 12 000 prostatic lobes and several combined clinicopathological variables, the absence of imaging characterization was the major point of weakness.
To date, the ideal predictive tool has yet to be described. However, in the modern era of precision surgery, we think that a model should encompass the surgical knowledge and techniques currently available.
Future developments will probably include three‐dimensional surgical navigation models displayed on the TilePro™ function of the robotic console (Intuitive Surgical Inc., Sunnyvale, CA, USA), based on the integration of MRI (for the number, size and location of disease) and predictive tools (to define the amount of ECE).
References
- Martini A, Gupta A, Lewis SC et al. Development and internal validation of a side‐specific, multiparametric magnetic resonance imaging‐based nomogram for the prediction of extracapsular extension of prostate cancer. BJU Int 2018; 122: 1025–33
- de Rooij M, Hamoen EH, Witjes JA, Barentsz JO, Rovers MM. Accuracy of magnetic resonance imaging for local staging of prostate cancer: a diagnostic meta‐analysis. Eur Urol 2016; 70: 233–45
- Morlacco A, Sharma V, Viers BR et al. The incremental role of magnetic resonance imaging for prostate cancer staging before radical prostatectomy. Eur Urol 2017; 71: 701–4
- Bleeker SE, Moll HA, Steyerberg EW et al. External validation is necessary in prediction research: a clinical example. J Clin Epidemiol 2003; 56: 826–32
- Tewari AK, Srivastava A, Huang MW et al. Anatomical grades of nerve sparing: a risk‐stratified approach to neural‐hammock sparing during robot‐assisted radical prostatectomy (RARP). BJU Int 2011; 108: 984–92
- Patel VR, Sandri M, Grasso AA et al. A novel tool for predicting extracapsular extension during graded partial nerve sparing in radical prostatectomy. BJU Int 2018; 121: 373–82
Editorial: A picture is worth a thousand words… but does it add utility to a nomogram to predict extraprostatic extension?
Martini et al. [1] ask whether adding in prostate MRI data to a preoperative nomogram can usefully aid in the decision to nerve‐spare on one or both sides in men undergoing radical prostatectomy, using a dataset of 829 positive prostate lobes in 561 men. The nomogram includes PSA, maximum ipsilateral Gleason grade, percentage core involvement, and presence of extracapsular extension (ECE) on MRI, although the percentage core involvement (< or >50%) was not found to be significant. Pathological ECE was noted in 142 (17.1%) of the lobes, and radiological suspicion of ECE was noted in 115 (14%) lobes.
The incorporation of MRI in the decision‐making process is to be welcomed. However, MRI only correctly predicted ECE in 57/142 (40.1%) cases, showing significant over‐ and under‐detection on MRI criteria alone. Nerve‐sparing was done in 78% of men, and 30 men had a positive surgical margin. The authors found the nomogram to have greater accuracy in predicting ECE than MRI alone, with an area under the curve for MRI alone of 68.83%, compared to 82.92% for the nomogram. The use of the nomogram to inform a decision to nerve‐spare, made independently for each side, is proposed.
We need to be clear about the different definitions that are being applied here. The MRI features used for assessing ECE, namely bulging/irregular margin, obliteration of the rectoprostatic angle, >1 cm capsular abutment, and neurovascular bundle invasion, set a somewhat high threshold, which we would expect to correlate with significant histological burden and ECE. The exact pathological definition of ECE is not described by the authors and so presumably includes presence of any cancer outside the surgical capsule, whilst the presence of a positive surgical margin is defined as any tumour touching an inked margin. This difference in the threshold for radiological and pathological significance of ECE has been noted by others [2]. In addition, there is some discussion of the long‐term clinical significance of a positive surgical margin of <3 mm [3], although both ECE and PSM are recognised as predictors of recurrence.
Even given this discrepancy in definitions, there are other possible reasons why MRI was less predictive than might be expected [4]. The majority (76%) of the MRI scans were done after biopsy, which is known to reduce the accuracy of MRI, resulting in both under‐ and over‐staging. These post‐biopsy effects can persist for some considerable time, often past the 4 week post‐biopsy recovery period used as the minimum in this series, and in many institutions [5]. Differences in prevalence of pathological ECE (17% in this series [1] vs 32.4% in the series reported by Gaunay et al. [4]) could also affect the performance characteristics of MRI for staging.
An alternative to the preoperative nomogram approach is the use of techniques such as neurovascular structure‐adjacent frozen‐section examination (NeuroSAFE) [6]. This allows an intraoperative decision on the extent of excision, based on frozen‐section examination, and it has been shown to increase the ability to nerve‐spare, with associated improved functional outcomes, whilst reducing positive surgical margins. However, it does have significant cost implications and is not widely available.
It makes sense to use preoperative MRI, currently widely recommended for staging, in combination with clinical parameters, to maximise the use of nerve‐sparing to favour functional outcomes, whilst minimising positive surgical margins. Martini et al. [1] present a nomogram based on readily available parameters, which could be readily adopted in the routine setting. The move towards MRI before first biopsy is likely to give us more accurate imaging data, which should help us to further refine the decision to nerve‐spare for men undergoing radical prostatectomy.
References
- Martini A, Gupta A, Lewis S et al. Development and internal validation of a side‐specific, multiparametric magnetic resonance imaging‐based nomogram for the prediction of extracapsular extension of prostate cancer. BJU Int 2018; 122: 1025–33
-
McEvoy SH, Raeside MC, Chaim J, Ehdaie B, Akin O. Preoperative prostate MRI: a road map for surgery. AJR Am J Roentgenol 2018; Jun 12: W1–9.
- Dev HS, Wiklund P, Patel V et al. Surgical margin length and location affect recurrence rates after robotic prostatectomy. Urol Oncol 2015; 33: 109.e7‐13
- Gaunay GS, Patel V, Shah P et al. Multi‐parametric MRI of the prostate: factors predicting extracapsular extension at the time of radical prostatectomy. Asian J Urol 2017; 4: 31–6
- Latifoltojar A, Dikaios N, Ridout A et al. Evolution of multi‐parametric MRI quantitative parameters following transrectal ultrasound‐guided biopsy of the prostate. Prostate Cancer Prostatic Dis 2015; 18: 343–51
- Mirmilstein G, Rai BP, Gbolahan O et al. The neurovascular structure‐adjacent frozen‐section examination (NeuroSAFE) approach to nerve sparing in robot‐assisted laparoscopic radical prostatectomy in a British setting ‐ a prospective observational comparative study. BJU Int 2018; 121: 854–62
Video: Development and internal validation of a side‐specific, mpMRI‐based nomogram for the prediction of extracapsular extension of PCa
Development and internal validation of a side‐specific, multiparametric magnetic resonance imaging‐based nomogram for the prediction of extracapsular extension of prostate cancer
Abstract
Objectives
To develop a nomogram for predicting side‐specific extracapsular extension (ECE) for planning nerve‐sparing radical prostatectomy.
Materials and Methods
We retrospectively analysed data from 561 patients who underwent robot‐assisted radical prostatectomy between February 2014 and October 2015. To develop a side‐specific predictive model, we considered the prostatic lobes separately. Four variables were included: prostate‐specific antigen; highest ipsilateral biopsy Gleason grade; highest ipsilateral percentage core involvement; and ECE on multiparametric magnetic resonance imaging (mpMRI). A multivariable logistic regression analysis was fitted to predict side‐specific ECE. A nomogram was built based on the coefficients of the logit function. Internal validation was performed using ‘leave‐one‐out’ cross‐validation. Calibration was graphically investigated. The decision curve analysis was used to evaluate the net clinical benefit.
Results
The study population consisted of 829 side‐specific cases, after excluding negative biopsy observations (n = 293). ECE was reported on mpMRI and final pathology in 115 (14%) and 142 (17.1%) cases, respectively. Among these, mpMRI was able to predict ECE correctly in 57 (40.1%) cases. All variables in the model except highest percentage core involvement were predictors of ECE (all P ≤ 0.006). All variables were considered for inclusion in the nomogram. After internal validation, the area under the curve was 82.11%. The model demonstrated excellent calibration and improved clinical risk prediction, especially when compared with relying on mpMRI prediction of ECE alone. When retrospectively applying the nomogram‐derived probability, using a 20% threshold for performing nerve‐sparing, nine out of 14 positive surgical margins (PSMs) at the site of ECE resulted above the threshold.
Conclusion
We developed an easy‐to‐use model for the prediction of side‐specific ECE, and hope it serves as a tool for planning nerve‐sparing radical prostatectomy and in the reduction of PSM in future series.