Article of the week: Going solo: using ultrasonography alone to guide PCNL
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by prominent members of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
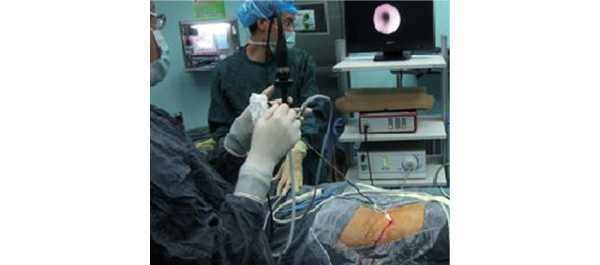
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr Yan and colleagues of ultrasonography-guided percutaneous nephrolithotomy.
If you only have time to read one article this week, it should be this one.
Percutaneous nephrolithotomy guided solely by ultrasonography: a 5-year study of >700 cases
Song Yan, Fei Xiang and Song Yongsheng
Division of Urology, Sheng Jing Hospital, China Medical University, Shenyang, China
OBJECTIVE
• To evaluate the safety and efficacy of percutaneous nephrolithotomy (PCNL) solely guided by ultrasonography (US).
PATIENTS AND METHODS
• From May 2007 to July 2012, 705 24-F-tract PCNL procedures were performed (679 patients, of whom 26 had bilateral stones).
• Calyceal puncture and dilatation were performed under US guidance in all cases.
• The procedure was evaluated for access success, length of postoperative hospital stay, complications (modified Clavien system), stone clearance and the need for auxiliary treatments.
RESULTS
• The mean (sd) operating time was 66 (25) min, with a mean (sd) postoperative hospital stay of 3.98 (1.34) days.
• The patients experienced a mean (sd) haemoglobin level decrease of 2.24 (2.02) g/day and the overall stone-free rate at 4 weeks after surgery was 92.6% in patients with a single calculus and 82.9% in patients with staghorn or multiple calculi.
• Auxiliary treatments, including shockwave lithotripsy in 52 patients, re-PCNL in 41 patients and ureteroscopy in 18 patients, were performed 1 week after the primary procedure in 111 (15.7%) cases for residual stones >4 mm in size.
• The sensitivities of intra-operative US-guidance and flexible nephroscopy for detecting significant residual stones and clinically insignificant residual fragments were 95.3 and 89.1%, respectively.
• There were 94 grade 1 (13.3%), 17 grade 2 (2.4%), and two grade 3 (0.3%) complications, but there were no grade 4 or 5 complications.
CONCLUSION
• Total US-guided PCNL is safe and convenient, and may be performed without any major complications and with the advantage of preventing radiation hazards and damage to adjacent organs.
Read Previous Articles of the Week