Archive for year: 2015
Article of the Week: Predicting pathological outcomes in patients undergoing RARP for high-risk prostate cancer
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Firas Abdollah, discussing his paper.
If you only have time to read one article this week, it should be this one.
Predicting Pathologic Outcomes in Patients Undergoing Robot-Assisted Radical Prostatectomy for High Risk Prostate Cancer: A Preoperative Nomogram
OBJECTIVE
To identify which high-risk patients with prostate cancer may harbour favourable pathological outcomes at radical prostatectomy (RP).
PATIENTS AND METHODS
We evaluated 810 patients with high-risk prostate cancer, defined as having one or more of the following: PSA level of >20 ng/mL, Gleason score ≥8, clinical stage ≥T2c. Patients underwent robot-assisted RP (RARP) with pelvic lymph node dissection, between 2003 and 2012, in one centre. Only 1.6% (13/810) of patients received any adjuvant treatment. Favourable pathological outcome was defined as specimen-confined disease (SCD; pT2–T3a, node negative, and negative surgical margins) at RARP-specimen. Logistic regression models were used to test the relationship among all available predicators and harbouring SCD. A logistic regression coefficient-based nomogram was constructed and internally validated using 200 bootstrap resamples. Kaplan–Meier method estimated biochemical recurrence (BCR)-free and cancer-specific mortality (CSM)-free survival rates, after stratification according to pathological disease status.
RESULTS
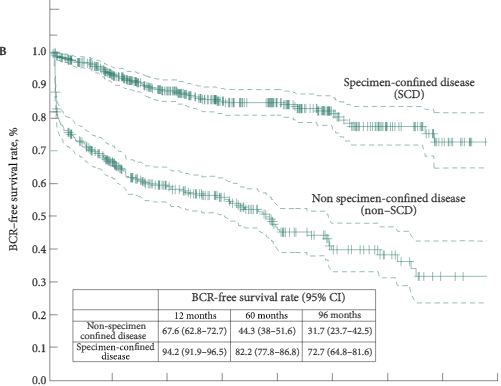
Overall, 55.2% patients harboured SCD at RARP. At multivariable analysis, PSA level, clinical stage, primary/secondary Gleason scores, and maximum percentage tumour quartiles were all independent predictors of SCD (all P < 0.04). A nomogram based on these variables showed 76% discrimination accuracy in predicting SCD, and very favourable calibration characteristics. Patients with SCD had significantly higher 8-year BCR- (72.7% vs 31.7%, P < 0.001) and CSM-free survival rates (100% vs 86.9%, P < 0.001) than patients with non-SCD.
CONCLUSIONS
We developed a novel nomogram predicting SCD at RARP. Patients with SCD achieved favourable long-term BCR- and CSM-free survival rates after RARP. The nomogram may be used to support clinical decision-making, and aid in selection of patients with high-risk prostate cancer most likely to benefit from RARP.
Editorial: More Nomograms or Better Lymph node dissection – What do we need in Prostate Cancer?
The publication of nomograms to predict radical prostatectomy (RP) outcome using preoperative parameters were important steps in urological oncology. Abdollah et al. [1], in this issue of BJU International, present a new nomogram to predict specimen-confined disease (SCD; pT2–3a, pN0 R0) in men with high-risk prostate cancer undergoing pelvic lymph node dissection (PLND) and robot-assisted RP (RARP). They used statistical logistic regression to measure the impact of various preoperatively available clinicopathological parameters on the likelihood of pathological outcome and tumour recurrence. The final nomogram accurately identified SCD (pT2–3a, pN0 R0) in 76% of the patients. It is intuitive that these patients have good long-term oncological outcomes after surgery. Consequently, Abdollah et al. found excellent 8-year cancer-specific survival rates in these patients. Because nomograms provide individualised risk prediction for patients in an easily applicable manner, they have become very popular among clinicians. Nomograms are now being applied for almost every aspect of prostate cancer. These are freely available and both patients and physicians are encouraged to use them.
Although nomograms undoubtedly have improved our perspective of disease behaviour and individual patient prediction, several key questions remain. First, how good are the input data to a nomogram? Abdollah et al. [1] evaluated 810 patients with high-risk prostate cancer treated in a single large centre between 2003 and 2012. Impressively, more than half of the patients (55%) harboured SCD at RARP. Such a high chance of having SCD will probably encourage many physicians and patients to choose surgery, even without using a nomogram, because this approach may avoid the need for hormonal treatment, which is obligatory for radiation therapy in high-risk prostate cancer. Second, is the predictive accuracy safe within clinical practice? Most nomograms using clinicopathological data generate predictive accuracies within the range of 75–90% (including the nomogram presented by Abdollah et al. [1]). It is of special importance to consider that 64/447 (14%) of the patients with SCD in the series reported by Abdollah et al. [1] received salvage treatment, which was initiated after a median (interquartile range, IQR) of 4.8 (1.4–9.3) months, and the indication to initiate this salvage therapy was PSA recurrence. Obviously, these patients did not have specimen confined disease and were misclassified. In this case, one might postulate a persistence of nodal disease, given an inadequate extent of PLND. Abdollah et al. [1] reported on a median (IQR) of 5 (3.0–11.0) lymph nodes removed.
In their landmark paper on extended PLND (ePLND) in cadavers, Weingartner et al. [2] demonstrated that a mean lymph node yield of 20 serves as a guideline for sufficient ePLND. More than 10 years ago, Heidenreich et al. [3] reported on a 15% higher rate of lymph node metastasis detection when comparing ePLND with the standard LND (obturator). Bader et al. [4] provided further evidence that an ePLND is needed to provide adequate clinical staging and potential therapeutic benefit. Of 365 patients with clinically localised prostate cancer, 88 (24%) had positive lymph nodes. In this series, a pelvic LND that spared the internal iliac bed would have left 58% of patients with positive nodes with residual disease and 19% would have been incorrectly staged as lymph node-negative for cancer. These data were recently confirmed by several authors when analysing retrospective series. Furthermore, Seiler et al. [5] updated their series of 88 patients and recently reported on the long-term outcome after a median follow-up of 15.6 years. They showed that 18% of those patients with one positive node remained biochemical recurrence free, 28% showed biochemical recurrence only, and 54% had clinical progression. Of these 39 patients, 57% never required deferred androgen-deprivation therapy. In contrast, patients with multiple positive nodes are likely to experience rapid progression and, thus, may benefit from early adjuvant therapies. International clinical practice guidelines recommend the performance of an anatomically ePLND at RP in men with high-risk prostate cancer, for both staging and therapeutic purposes.
Nowadays, most urologists claim to perform an ePLND. However, a recent analysis among 50 671 men who were surgically treated with RP from 2010 to 2011 in the USA showed that, overall, only 69.3% of the high-risk patients underwent concomitant PLND [6]. Surgical approach and hospital characteristics were associated with treatment with PLND and detection of lymph node metastasis. More specifically, patients with prostate cancer undergoing open RP or surgically treated at high-volume centres were more likely to undergo PLND than those undergoing RARP or surgically treated at low-volume centres.
Despite the strong evidence that ePLND positively affects survival in men with limited lymph node involvement, this procedure is not commonly performed. The reasons for this are multiple and include expertise, stage migration and functional and oncological outcomes, as well as economics and the introduction of laparoscopic and laparoscopic RARP. However, this is no reason not to offer the patient, if possible, an operation which has the highest chance of cure
Video: Predicting pathological outcomes in patients undergoing RARP for high-risk prostate cancer: A Preoperative Nomogram
Predicting Pathologic Outcomes in Patients Undergoing Robot-Assisted Radical Prostatectomy for High Risk Prostate Cancer: A Preoperative Nomogram
OBJECTIVE
To identify which high-risk patients with prostate cancer may harbour favourable pathological outcomes at radical prostatectomy (RP).
PATIENTS AND METHODS
We evaluated 810 patients with high-risk prostate cancer, defined as having one or more of the following: PSA level of >20 ng/mL, Gleason score ≥8, clinical stage ≥T2c. Patients underwent robot-assisted RP (RARP) with pelvic lymph node dissection, between 2003 and 2012, in one centre. Only 1.6% (13/810) of patients received any adjuvant treatment. Favourable pathological outcome was defined as specimen-confined disease (SCD; pT2–T3a, node negative, and negative surgical margins) at RARP-specimen. Logistic regression models were used to test the relationship among all available predicators and harbouring SCD. A logistic regression coefficient-based nomogram was constructed and internally validated using 200 bootstrap resamples. Kaplan–Meier method estimated biochemical recurrence (BCR)-free and cancer-specific mortality (CSM)-free survival rates, after stratification according to pathological disease status.
RESULTS
Overall, 55.2% patients harboured SCD at RARP. At multivariable analysis, PSA level, clinical stage, primary/secondary Gleason scores, and maximum percentage tumour quartiles were all independent predictors of SCD (all P < 0.04). A nomogram based on these variables showed 76% discrimination accuracy in predicting SCD, and very favourable calibration characteristics. Patients with SCD had significantly higher 8-year BCR- (72.7% vs 31.7%, P < 0.001) and CSM-free survival rates (100% vs 86.9%, P < 0.001) than patients with non-SCD.
CONCLUSIONS
We developed a novel nomogram predicting SCD at RARP. Patients with SCD achieved favourable long-term BCR- and CSM-free survival rates after RARP. The nomogram may be used to support clinical decision-making, and aid in selection of patients with high-risk prostate cancer most likely to benefit from RARP.
Article of the Week: Does timing matter in postoperative RT for patients at high-risk of recurrence after RP?
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Peter Carroll, discussing his paper.
If you only have time to read one article this week, it should be this one.
Postoperative radiation therapy for patients at high-risk of recurrence after radical prostatectomy: does timing matter?
OBJECTIVE
To evaluate among radical prostatectomy (RP) patients at high-risk of recurrence whether the timing of postoperative radiation therapy (RT) (adjuvant, early salvage with detectable post-RP prostate-specific antigen [PSA], or ‘late’ salvage with a PSA level of >1.0 ng/mL) is significantly associated with overall survival (OS), prostate-cancer specific survival or metastasis-free survival, in a longitudinal cohort.
PATIENTS AND METHODS
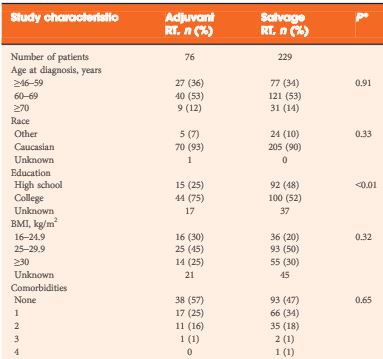
Of 6 176 RP patients in the Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE), 305 patients with high-risk pathological features (margin positivity, Gleason score 8–10, or pT3–4) who underwent postoperative RT were examined, either in the adjuvant (≤6 months after RP with undetectable PSA levels, 76 patients) or salvage setting (>6 months after RP or pre-RT PSA level of >0.1 ng/mL, 229 patients). Early (PSA level of ≤1.0 ng/mL, 180 patients) or late salvage RT (PSA level >1.0 ng/mL, 49 patients) was based on post-RP, pre-RT PSA level. Multivariable Cox regression examined associations with all-cause mortality and prostate cancer-specific mortality and/or metastases (PCSMM).
RESULTS
After a median of 74 months after RP, 65 men had died (with 37 events of PCSMM). Adjuvant and salvage RT patients had comparable high-risk features. Compared with adjuvant, salvage RT (early or late) had an increased association with all-cause mortality (hazard ratio [HR] 2.7, P = 0.018) and with PCSMM (HR 4.0, P = 0.015). PCSMM-free survival differed by further stratification of timing, with 10-year estimates of 88%, 84%, and 71% for adjuvant, early salvage, and late salvage RT, respectively (P = 0.026). For PCSMM-free survival and OS, compared with adjuvant RT, late salvage RT had statistically significantly increased risk; however, early salvage RT did not.
CONCLUSION
This analysis suggests that patients who underwent early salvage RT with PSA levels of <1.0 ng/mL may have comparable metastasis-free survival and OS compared with adjuvant RT; however, late salvage RT with a PSA level of >1.0 ng/mL is associated with worse clinical outcomes.
Editorial: Does a positive margin always mandate adjuvant radiotherapy?
The appropriate treatment for clinically localized prostate cancer continues to generate controversy. For men with low grade disease it is unclear whether surgery or radiation therapy provides a survival advantage over active surveillance, and among men with high grade disease it is unclear how many derive a substantial benefit from either intervention. No trial has yet to compare surgery and radiation with observation, but the recent update of the Scandinavian Prostate Cancer Group 4 study suggests that radical prostatectomy provides a significant survival advantage for younger men with intermediate grade disease [1].
Unfortunately, many men undergoing radical prostatectomy are not cured of their disease. The Scandinavian Prostate Cancer Group 4 study has shown that as many as 26% of men undergoing surgery developed distant metastases and 18% died from their disease after a median follow-up of 13 years. For this reason many clinicians recommend additional radiation therapy for those men undergoing surgery who are at high risk of disease recurrence. Three randomized trials now support the use of radiation therapy in this setting. Two have shown lower rates of biochemical progression and one has shown improved distant metastases-free survival and overall survival [2-4]. These trials compared the use of adjuvant radiation therapy with observation. Some clinicians, however, are reluctant to refer patients for radiation therapy because of concerns about its potential impact on quality of life. This is especially true for those patients who have yet to show any evidence of biochemical recurrence.
In a manuscript published in this month’s BJUI, Hsu et al. [5] have turned to a large national prostate cancer registry that has accrued men with newly diagnosed prostate cancer since 1995. They evaluated the long-term outcomes of these men to gain insights into whether a delay in the initiation of radiation therapy compromises survival. Their findings suggest that delaying the initiation of radiation therapy until there is evidence of biochemical recurrence does not seriously compromise long-term outcomes and avoids radiation in some men who are never destined to have disease progression.
The authors are appropriately cautious with their conclusions and clearly recognize the limitations of a non-randomized study. In a registry study it is impossible to control adequately for selection biases. Men receiving adjuvant therapy had no evidence of biochemical recurrence at the time radiation was started. This group of men included both men who were destined to have disease progression and men who were destined to maintain an undetectable PSA. This differs from the men receiving salvage radiation therapy. All men receiving salvage radiation had evidence of disease progression and therefore their tumour burden and their long-term prognosis was probably worse when compared with men receiving adjuvant therapy. Despite this selection bias, men initiating salvage radiation when their postoperative PSA level was still <1.0 ng/mL had similar long-term outcomes when compared with the men receiving adjuvant radiation. Men with postoperative PSA levels >1.0 ng/mL had a much higher risk of aggressive disease and a worse outcome.
Ideally, the question about the timing of postoperative radiation would be subjected to a randomized trial. Until then, the information provided by Hsu et al. provides strong clinical support for a practical approach to the question of who should receive postoperative radiation. Men who are clearly at high risk of disease progression, which includes men with Gleason 8–10 disease and those with extensive margin positive disease and seminal vesicle invasion, should probably receive adjuvant radiation therapy as soon as they have recovered from surgery. For men with Gleason 7 disease or those men who have focal margin-positive disease it may make sense to monitor postoperative PSA levels closely and refer men for postoperative radiation when there is evidence of biochemical progression and before the PSA level reaches 1.0 ng/mL. This approach would spare some men the need for additional treatment and would defer treatment for many years in others. Men who are eventually found to have biochemical recurrence should feel reasonably comfortable that the delay in initiating radiation therapy is unlikely to have caused any significant compromise of their long-term outcome and probably improved their quality of life.
Large case series analyses frequently have selection biases that confound conclusions. In this instance the authors have cautiously interpreted a large community-based registry to gain a valuable insight into the management of localized prostate cancer. Their analysis provides appropriate support for their conclusions.
Video: Postoperative RT for patients at high-risk of recurrence after RP: does timing matter?
Postoperative radiation therapy for patients at high-risk of recurrence after radical prostatectomy: does timing matter?
OBJECTIVE
To evaluate among radical prostatectomy (RP) patients at high-risk of recurrence whether the timing of postoperative radiation therapy (RT) (adjuvant, early salvage with detectable post-RP prostate-specific antigen [PSA], or ‘late’ salvage with a PSA level of >1.0 ng/mL) is significantly associated with overall survival (OS), prostate-cancer specific survival or metastasis-free survival, in a longitudinal cohort.
PATIENTS AND METHODS
Of 6 176 RP patients in the Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE), 305 patients with high-risk pathological features (margin positivity, Gleason score 8–10, or pT3–4) who underwent postoperative RT were examined, either in the adjuvant (≤6 months after RP with undetectable PSA levels, 76 patients) or salvage setting (>6 months after RP or pre-RT PSA level of >0.1 ng/mL, 229 patients). Early (PSA level of ≤1.0 ng/mL, 180 patients) or late salvage RT (PSA level >1.0 ng/mL, 49 patients) was based on post-RP, pre-RT PSA level. Multivariable Cox regression examined associations with all-cause mortality and prostate cancer-specific mortality and/or metastases (PCSMM).
RESULTS
After a median of 74 months after RP, 65 men had died (with 37 events of PCSMM). Adjuvant and salvage RT patients had comparable high-risk features. Compared with adjuvant, salvage RT (early or late) had an increased association with all-cause mortality (hazard ratio [HR] 2.7, P = 0.018) and with PCSMM (HR 4.0, P = 0.015). PCSMM-free survival differed by further stratification of timing, with 10-year estimates of 88%, 84%, and 71% for adjuvant, early salvage, and late salvage RT, respectively (P = 0.026). For PCSMM-free survival and OS, compared with adjuvant RT, late salvage RT had statistically significantly increased risk; however, early salvage RT did not.
CONCLUSION
This analysis suggests that patients who underwent early salvage RT with PSA levels of <1.0 ng/mL may have comparable metastasis-free survival and OS compared with adjuvant RT; however, late salvage RT with a PSA level of >1.0 ng/mL is associated with worse clinical outcomes.
The second joint academic meeting of the Sri Lankan and British Associations of Urological Surgery (SLAUS & BAUS)
The inaugural international joint meeting of BAUS and SLAUS was held two years ago. The second joint meeting has just finished in Colombo, bringing together British and Sri Lankan urologists. We were also joined by excellent Chinese and Indian colleagues.
The meeting commenced on Monday 2nd November with a series of urological workshops. These started with an excellent laparoscopic workshop at Colombo South Teaching Hospital, led by Gordon Kooiman (King’s, UK), Wei Wang, Zhu Gang (Bejing) and Srinath Chandrasekera (Sri Lanka).
The College of Surgeons of Sri Lanka was the chosen venue for the second day of the pre-congressional sessions. This kicked off with a trans-world MDT, with John Kelleher (UK), Gordon Kooiman (UK), Mark Speakman (President of BAUS), Archana Fernando (Guy’s and St Thomas’ Hospitals, London), Sanchia Goonewardene (University of Warwick), Ranga Wickramarachi (National Hospital of Sri Lanka) and Niroshen Seneviratne, (Sri Jayawardenapura, Sri Lanka). Fifteen complex cancer cases were presented, ranging from prostate and bladder cancer to complex renal cases. The intellectual sparks flew as each side vigorously debated their management of each patient, with input from Chinese Professors Zhu Gang and Wei Wang. The MDT was wonderfully organised by Dr Ranga Wickramarachi, who brought together both faculties, with solid science and learning on both sides.
The afternoon was led by Mr Julian Shah (University College London), who presented on medico-legal issues and communication skills, with input from Sri Lankan doctors. There are an ever increasing number of medico-legal situations clinicians may find themselves in, and this workshop provided the tools for how to manage them. Also noteworthy were the acting skills of Dr Manjula Herath (Kandy Hospital, Sri Lanka) and his colleagues, who deserved an Oscar for the excellent case scenarios they enacted as a background for a critique of their communication skills. On a more serious note, these clearly highlighted issues that are becoming more and more significant in today’s practice.
The third day of the pre-congressional sessions was a trip to Galle in the south of the island for a joint meeting with the Galle Medical Association. A 6am start was complemented by teaching on the neuropathic bladder by Ms Jean Macdonald and Mr Julian Shah, as well as a workshop on penile diseases from Mr Suks Minas at the Jetwing Lighthouse hotel. There was also teaching from Galle medical personnel, notably Kareen Hareen on haematuria. Additionally, there was a lecture on LUTS/BOO from Mr Speakman, and wise lessons to all trainees present on the validity of BPH treatment. A wonderful lunch was served, with chances to interact with Sri Lankan trainees and to clearly see differences in training in both countries – although we are not that dissimilar. A relaxed afternoon beckoned, including a wonderful tour of the ancient Portuguese Galle fort and its scenery. This was followed by afternoon tea at the Closernberg Hotel, Galle.
The next day brought live surgery at Lanka Hospital, conducted by Julian Shah, and Suks Minhas (University College London), with a focus on female and functional urology. A complicated ureteric strictures managed by pyeloplasty and a complex female urethral stricture were demonstrated with live surgery. Additionally, there were video operative lectures by EAU Secretary General Professor Chris Chapple (Royal Hallamshire Hospital, Sheffield), on urethroplasty; valuable lessons for all trainees.
There was also a visit to Sri Jayawardenapura hospital from the Faculty. It was brilliant to see Sri Lankan medicine in practice, with lessons to be learnt by all BAUS faculty members. Afterwards a workshop on trauma occurred at the Faculty of Medicine, University of Sri Jayardenapura, composed of all Faculty members. The best lesson learnt was how to manage renal trauma. This was followed by a hands-on skills for ureteric reconstruction. The course, run by Peter Thompson, had been started 20 years before by Prof. Harold Ellis at RCS England. This was run by Mr Thompson, Ms Goonewardene and Prof. Wang (China). It was considered a fantastic opportunity for all trainees, with hands-on experience of anastomoses of the pig urinary system. Its success was justified the next day when, in practice, a trainee was called upon to manage a ureteric injury.
A beautiful inauguration ceremony in front of 200 people was conducted that evening at Kings Court, Cinnamon Lakeside Hotel, with traditional Kandian dancing and lighting of the oil lamp. This was followed by inauguration speeches, given by Prof. Satish Goonesinghe (Colombo), Prof. Chris Chapple (EAU), and Mr Mark Speakman (BAUS). The evening ended with entertainment from Kandian dancers, and singing from Prof. J. Shah, Prof. S. Fonseka and Mr J. Kelleher– the rock band was aptly named ‘The Professors.’
The next day, the full congress kicked off, with a presentation from Mr Thompson on the history of British urology. The audience learned about great legends, including Malcolm Coptcoat, pioneer of laparoscopic surgery at King’s College London. The next section was on urolithiasis, started by Ms S. Goonewardene on metabolic stone analysis, Ms J. Macdonald (North Middlesex Hospital) on PCNL, and finally from Dr Ranga Wickramararchi on open stone surgery. The learning outcomes demonstrated to trainees the importance of being a well-trained general urologist prior to sub speciality training.
The next section was brightened by Mark Speakman, President of BAUS, talking on surgeons’ outcome data — a really valid subject as this can greatly impact surgical practice. Training issues as part of this were also highlighted. At the end of the day, this can also be used as a continuous assessment tool to improve practice. This was followed by Prof. C. Chapple talking on OAB, a complex subject to manage. There was great interaction between trainees and Faculty, a wonderful learning experience.

Mark Speakman, Chris Chapple, Satish Goonesinghe and Majula Herath at the Inuguration ceremony
This was followed, after a lovely tea, by Julian Shah speaking on female voiding difficulties. This was very important to all present, as it clearly highlighted other factors that can affect bladder function. After that, Prof. Chapple spoke on advances in pharmacotherapeutic management of LUTS; valuable lessons for all present. Also presented were the potential complications or failures of TURP prostatectomy, highlighting the importance of good case selection. To complete this section, the sensitive bladder was reviewed by Dr Sanjay Pandey, (India).
After lunch there were registrar presentations, varying from renal cell carcinoma to paediatric urethral valves. The afternoon was completed by a detailed uro-oncology session, with presentations from Gordon Kooiman, Mark Speakman, Suks Minhas and John Kelleher, covering a range of oncological subjects.
Each speaker was presented with a beautiful silver plaque for their involvement. The ceremony concluded with an evening dinner aboard an arc in the Colombo wetlands. The meeting closed, and was clearly one of the most successful there had ever been, with the promise of returning in years to come with further joint BAUS/SLAUS meetings.
–Mark Speakman and Sanchia Goonewardene
Mark J Speakman
Consultant Urologist, Taunton & Somerset FNHST and President BAUS
Twitter: @Parabolics
Does presentation with metastatic prostate cancer matter?
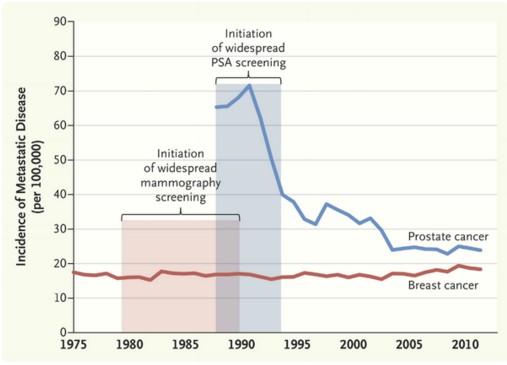
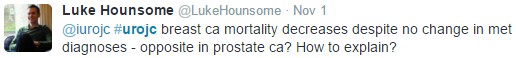
 November saw the return of the International Urology Journal Club #urojc on Twitter. The annual meetings of the World Congress for Endourology (#WCE2015) and Société Internationale D’Urologie (#SIU15) led to an October break for #urojc. This month’s discussion was based around a recent editorial in the New England Journal of Medicine by Welch et al on the effects of screening on the incidences of metastatic-at-diagnosis prostate and breast cancers. In the three days prior to the start of the discussion the editorial and it’s now well-known graph had been trending amongst medical Twitter users.
November saw the return of the International Urology Journal Club #urojc on Twitter. The annual meetings of the World Congress for Endourology (#WCE2015) and Société Internationale D’Urologie (#SIU15) led to an October break for #urojc. This month’s discussion was based around a recent editorial in the New England Journal of Medicine by Welch et al on the effects of screening on the incidences of metastatic-at-diagnosis prostate and breast cancers. In the three days prior to the start of the discussion the editorial and it’s now well-known graph had been trending amongst medical Twitter users.
The issue of PSA screening for prostate cancer has been a topic of debate amongst urologists for a number of years. PSA and DRE are first line for early detection of prostate cancer. Supporters of PSA screening argue that it leads to a significant fall in prostate cancer specific mortality. Many others believe there is insufficient evidence to support universal PSA screening given the risks of prostate biopsy and potential overtreatment of low risk prostate cancer.
The editorial presented data showing a significant fall in the number of patients first presenting with metastatic prostate cancer (advanced stage incidence) following the introduction of universal screening. However no effect was shown on similar data for breast cancer. Variations in disease dynamics were suggested to play a role.
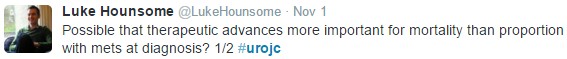
The conversation started on Sunday 1st November at 20:00 (GMT), marking the beginning of the fourth year of #urojc. The first questions centred around the reasons behind the trends seen in the graph. Being a urology journal club the conversation was based almost exclusively on the prostate cancer aspect of the editorial.
One suggestion for the discrepancy between the two cancers is that PSA is a better detector of metastatic disease, whilst mammography can only detect localised disease.
Based on incidence of metastatic prostate cancer, the article makes a convincing statement in support of universal PSA screening. However, a successful screening programme should result in a reduction in the incidence of advanced cancers, decreased advanced-stage incidence and reduced mortality. Leading to the question of whether looking solely at advanced-stage incidence is useful.
The importance of responsible treatment and active surveillance was mentioned early on.
One of the most important questions of the discussion: What impact and relevance does the image have? Views were polarised. Some contributors were cautious about drawing conclusions from the graph whilst others were satisfied that it justified PSA screening.
The article drew comparison between Halsted’s and Fisher’s descriptions of cancer progression. Halsted suggested cancer originates from a single site and spreads, whereas Fisher’s paradigm proposed that breast cancer is a systemic disease by the time it is detectable.
The United States Preventive Services Task Force (USPSTF) has recommended against universal screening of prostate cancer, suggesting the risks of testing outweighed the benefits. However, many believe this to be based on outdated evidence.
The Prostate, Lung, Colorectal and Ovarian (PLCO) Cancer Screening Trial results showed a 12% higher incidence of prostate in the screening arm versus control, with no difference in mortality. Yet, the European Randomized Study of Screening for Prostate Cancer (ERSPC) has shown screening to result in a 1.6 fold increase in prostate cancer with a 21% reduction in mortality.
The debate briefly discussed the morbidity and cost of metastatic disease.
The editorial certainly raised a number of interesting points. It seems the topic of universal PSA screening will continue to be debated. There is a significant benefit to screening in the prevention of metastatic prostate cancer. Whether this is due to differing disease dynamics or PSA being a better screening tool than mammography is as yet unclear.
One point we can all agree on is that increasing utilisation of active surveillance with timely biopsies is important in preventing overtreatment of low risk disease and identifying those at risk of disease progression for curative treatment.
Anthony Noah Urology Speciality Trainee, West Midlands, UK
Twitter: @antnoah