Editorial: The pursuit of purpose: reframing strategies to prevent physician burnout
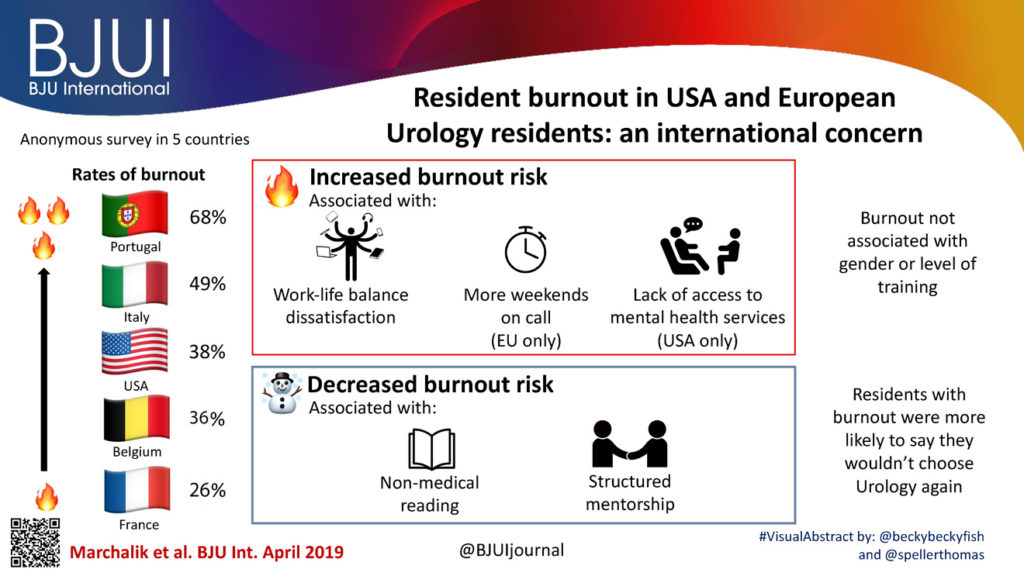
If there is one virtue that drives surgery residents to toil away in sterile, brightly lit operating rooms for extended hours for the best years of their life, it is the pursuit of purpose. However, these extended hours can also lead to what the WHO has now officially recognized as a medical condition: burnout. In a study in this issue of BJUI, Marchalik et al. [1] use qualitative analysis to elaborate on the prevalence and predictors of burnout among urology residents in the USA and in four European countries. Using an anonymous survey, the authors report a high prevalence of burnout in urology residents in both cohorts, with the European residents (44%) experiencing a higher burden than their US counterparts (38%). Given the recent focus, in the academic as well as general media, on the importance and severe implications of physician burnout, and the recognition of burnout as a disease by WHO, the timing of this publication for concrete organizational action seems propitious, especially since this analysis combines data from two continents with different institutional and educational frameworks, providing more granular data for a particularly immersive surgical specialty with a high rate of burnout.
Most recently, a cost–consequence analysis reported that physician burnout costs approximately $4.6 bn each year to the US healthcare system, with a cost of $7600 per‐physician‐per‐year at the institutional level resulting from reduced clinical productivity and turnover [2]. While addressing these economic losses from burnout is important from an organizational and health system point of view, focusing on these alone would be missing the larger picture. It is only when we consider the depersonalization, emotional drainage, and loss of professional and personal accomplishment associated with burnout that we begin to realize the scope of this epidemic. Deservedly, burnout is being recognized as a ‘moral injury’ [3]. And indeed, it is a moral injury: when physicians working under systems that betray their purpose as a healer, the damage is not only professional and systematic, but deeply personal as well.
The constant act of balancing competing demands – the financial interests of the healthcare institutions, looming litigations and ever‐changing documentation requirements – has undermined effective human interactions with patients and diminished the zeal that drives physicians to spend a major part of their youth in training. Journalist Diane Silver defines moral injury as ‘a deep soul wound that pierces a person’s identity, sense of morality, and relationship to society’ [3]. Except in the context of healthcare delivery, this injury extends to deterioration of relationships with patients and fellow physicians. Indeed, burnout among physicians has been demonstrated to be associated with suboptimal patient care [4], and the consequent inability to deliver high‐quality care because of health system deficiencies leads to decline in physician well‐being and professional dissatisfaction [5].
While the urgency of addressing physician burnout is obvious, this study by Marchalik et al. is also valuable as it highlights some of the practices that are protective, revealing lessons that can be implemented. The authors report that burnout was significantly lower among residents who sought mental health services and those who had access to structured mentorship. Unsurprisingly, those who had a caring environment experienced less depersonalization and emotional drainage. This is an instructive lesson for the residency programme directors: if they want their most important human resource to flourish, they need to start building supportive work environments. This could start with pairing interns and residents with dedicated and experienced faculty mentors; these initiatives would facilitate career coaching and provide space where residents feel comfortable seeking information on mental healthcare.
Interestingly, the authors also found a significant dose–response relationship between the number of non‐medical books residents read per month and decreased rates of burnout. This finding may surprise some healthcare administrators, who have routinely attempted to integrate ‘wellness’ and ‘mindfulness’ into clinical programmes to stimulate physician motivation, without much benefit. However, the positive relationship between non‐medical literature and medicine is an ancient one. Fortunately, in the last few decades, this relationship has witnessed a comeback and an increasing number of trainees are finding solace in their engagement with medical humanities and narrative medicine. These engagements have led to physicians developing emotional intelligence, empathy for patients and colleagues, and an opportunity to examine their role as healers [6]. This insight from the study should be another lesson for medical educators, who can encourage inclusion of reflections on life as a physician.
The epidemic of burnout among surgery residents requires immediate attention. Taking proactive action towards this is not only a matter of preventing economic loss or improving physician productivity, but an urgent ethical issue. All stakeholders – hospital administrators, healthcare policy‐makers, and regional physician leaders – must work together in developing inventive solutions to address the burnout epidemic. This will be essential to realizing the maximal potential of residency and reinstating purpose of clinical work.
References
- , , et al. Resident burnout in USA and European urology residents: an international concern. BJU Int 2019; 124: 349‐ 56
- , , et al. Estimating the attributable cost of physician burnout in the United States cost of physician burnout. Ann Intern Med 2019; 170: 784‐ 90
- , . Physicians aren’t ‘burning out.’ They’re suffering from moral injury. STAT News 2018. Available at: https://www.statnews.com/2018/07/26/physicians-not-burning-out-they-are-suffering-moral-injury/. Accessed May 29, 2019.
- , , , . Burnout and self‐reported patient care in an internal medicine residency program. Ann Intern Med 2002; 136: 358– 67
- , , et al. Factors affecting physician professional satisfaction and their implications for patient care, health systems, and health policy. Rand Health Q 2014; 3: 1
- . Literature & medicine: humanities at the heart of health care: a hospital‐based reading and discussion program developed by the Maine humanities council. Acad Med 2003; 78:963– 7