Posts
Article of the week: Cluster analysis of multiple chronic conditions associated with urinary incontinence among women in the USA
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation. There is also a new residents’ podcast focussing on this article.
If you only have time to read one article this week, it should be this one.
Cluster analysis of multiple chronic conditions associated with urinary incontinence among women in the USA
Abstract
Objective
To identify patterns of prevalent chronic medical conditions among women with urinary incontinence (UI).
Materials and Methods
We combined cross‐sectional data from the 2005–2006 to 2011–2012 US National Health and Nutrition Examination Surveys, and identified 3 800 women with UI and data on 12 chronic conditions. Types of UI included stress UI (SUI), urgency UI (UUI), and mixed stress and urgency UI (MUI). We categorized UI as mild, moderate or severe using validated measures. We performed a two‐step cluster analysis to identify patterns between clusters for UI type and severity. We explored associations between clusters by UI subtype and severity, controlling for age, education, race/ethnicity, parity, hysterectomy status and adiposity in weighted regression analyses.
Results
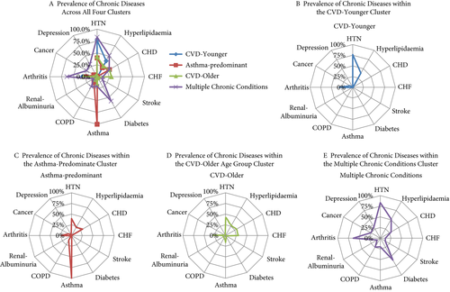
Eleven percent of women with UI had no chronic conditions. Among women with UI who had at least one additional condition, four distinct clusters were identified: (i) cardiovascular disease (CVD) risk‐younger; (ii) asthma‐predominant; (iii) CVD risk‐older; and (iv) multiple chronic conditions (MCC). In comparison to women with UI and no chronic diseases, women in the CVD risk‐younger (age 46.7 ± 15.8 years) cluster reported the highest rate of SUI and mild UI severity. In the asthma‐predominant cluster (age 51.5 ± 10.2 years), women had more SUI and MUI and more moderate UI severity. Women in the CVD risk‐older cluster (age 57.9 ± 13.4 years) had the highest rate of UUI, along with more severe UI. Women in the MCC cluster (age 61.0 ± 14.8 years) had the highest rates of MUI and the highest rate of moderate/severe UI.
Conclusions
Women with UI rarely have no additional chronic conditions. Four patterns of chronic conditions emerged with differences by UI type and severity. Identification of women with mild UI and modifiable conditions may inform future prevention efforts.
Residents’ podcast: Urinary continence recovery after radical prostatectomy
Maria Uloko is a Urology Resident at the University of Minnesota Hospital and Giulia Lane is a Female Pelvic Medicine and Reconstructive Surgery Fellow at the University of Michigan.
In this podcast they discuss the BJUI Article of the Week ‘Investigating the mechanism underlying urinary continence recovery after radical prostatectomy: effectiveness of a longer urethral stump to prevent urinary incontinence‘.
Investigating the mechanism underlying urinary continence recovery after radical prostatectomy: effectiveness of a longer urethral stump to prevent urinary incontinence
*Department of Integrative Cancer Therapy and Urology, Kanazawa University Graduate School of Medical Science, Kanazawa, Japan; †Department of Radiology, Kanazawa University School of Medicine, 13‐1 Takara‐machi, Kanazawa, Ishikawa 920‐8640, Japan
Abstract
Objective
To assess the chronological changes in urinary incontinence and urethral function before and after radical prostatectomy (RP), and to compare the findings of pelvic magnetic resonance imaging (MRI) before and after RP to evaluate the anatomical changes.
Patients and Methods
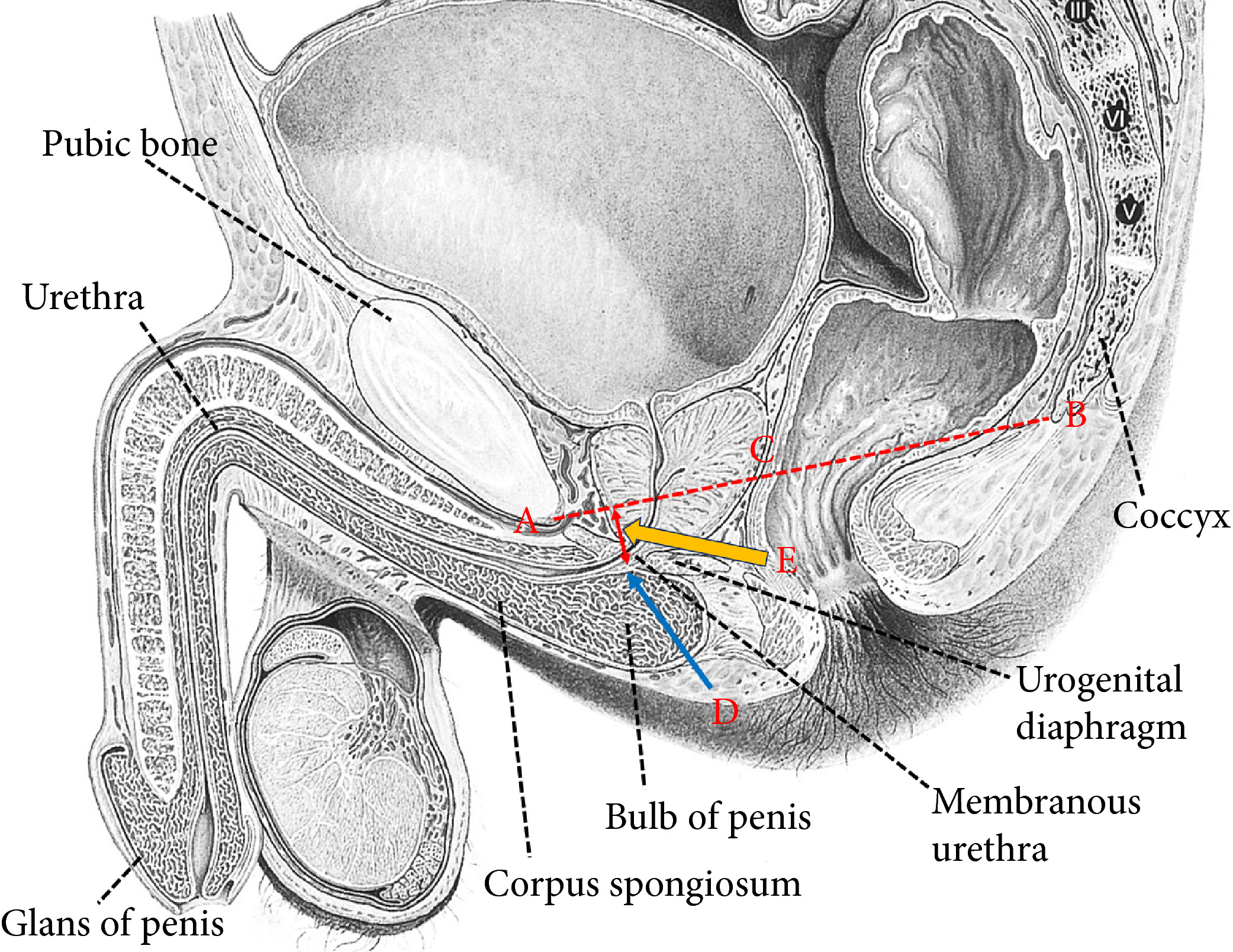
In total, 185 patients were evaluated with regard to the position of the distal end of the membranous urethra (DMU) on a mid‐sagittal MRI slice and urethral sphincter function using the urethral pressure profilometry. The patients also underwent an abdominal leak point pressure test before RP and at 10 days and 12 months after RP. The results were then compared with the chronological changes in urinary incontinence.
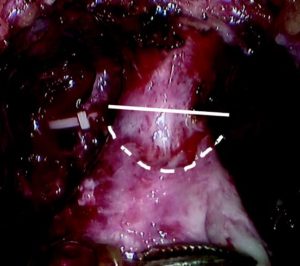
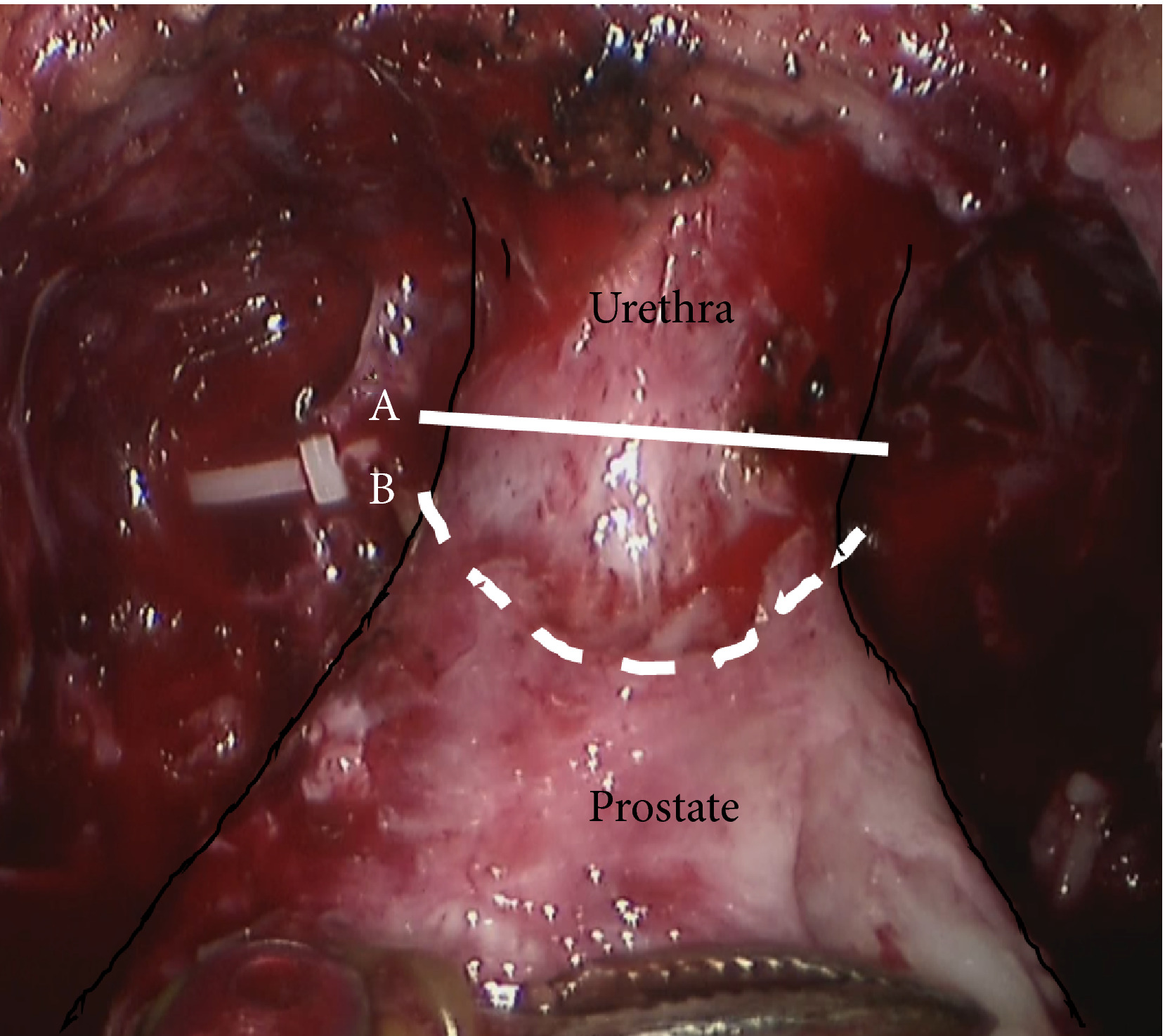
Fig. 1 Intraoperative view of the apex of the prostate transection line between the urethra and prostate at the normal (straight line) and long urethral stump (dashed line) positions.
Results
The MRI results showed that the DMU shifted proximally to an average distance of 4 mm at 10 days after RP and returned to the preoperative position at 12 months after RP. Urethral sphincter function also worsened 10 days after RP, with recovery after 12 months. The residual length of the urethral stump and urinary incontinence were significantly associated with the migration length of the DMU at 10 days after RP. The residual length of the urethral stump was a significant predictor of urinary incontinence after RP.
Conclusion
This is the first study to elucidate that the slight vertical repositioning of the membranous urethra after RP causes chronological changes in urinary incontinence. A long urethral residual stump reduces urinary incontinence after RP.
BJUI Podcasts now available on iTunes, subscribe here https://itunes.apple.com/gb/podcast/bju-international/id1309570262
Editorial: Towards an individualized approach for predicting post‐prostatectomy urinary incontinence: the role of nerve preservation and urethral stump length
Traditionally, MRI of the prostate has been mainly applied in the diagnosis and staging of prostate cancer. Kadono et al. [1] used pre‐ and postoperative pelvic MRI to assess the repositioning of the urethra 10 days and 12 months after prostatectomy, hypothesizing that these alterations could correlate with urinary incontinence and urethral function. Recent MRI measurements of anatomical structures of the pelvic floor, such as membranous urethral length and inner levator distance, were found to be independent predictors of early continence recovery at 12 months after prostatectomy [2] A meta‐analysis has also shown a strong correlation between membranous urethral length and continence recovery at 3‐, 6‐ and 12‐month follow‐up [3] Kadono et al. [1] add another metric to the pelvic floor dimensions that may help predict continence. Cranial migration of the lower end of the membranous urethra early after prostatectomy was associated with urinary incontinence and urinary sphincter function, as objectively assessed by urethral pressure profile. Interestingly, return of the membranous urethra to the more distal preoperative position after 12 months was associated with improvement in continence. In a multivariate model, urethral stump length was a strong predictor of continence outcome at 10 days as well as 12 months after prostatectomy. This observation suggests that urethral length may partly improve post-prostatectomy continence through better compression of the membranous urethra in the pelvic floor membrane rather than through transfer of the intra‐abdominal pressure onto the intra‐abdominally located urethra. If confirmed, this observation may imply that more cranial fixation of the bladder neck in a more intra‐abdominal position may not necessarily improve continence after prostatectomy, in line with data from randomized controlled studies comparing median fibrous raphe reconstruction with standard anastomosis that failed to show a benefit [4,5].
Besides anatomical location, innervation of the proximal urethra is important for post-prostatectomy continence [6]. Kadono et al. found that nerve preservation was an independent predictor of early and long‐term continence outcome, with a b value similar to that of urethral stump length at 12‐month follow‐up. To improve post-prostatectomy continence outcome, proper patient selection seems crucial. In the era of personalized medicine, MRI could be a valuable tool to assess preoperatively the risks of postoperative urinary incontinence and counsel patients accordingly. Avoiding prostatectomy in men with short preoperative membranous urethral length may be an important approach for improving outcome, in particular in light of the fact that many attempts to surgically correct anatomical alignment of the pelvic floor have not clearly improved continence outcome. If surgery is considered, nerve preservation should be performed where possible to improve continence.
Henk G. van der Poel and Nikos Grivas
Department of Urology, Netherlands Cancer Institute, Amsterdam, The Netherlands
References
- Kadono Y, Nohara T, Kawaguchi S et al. Investigating the mechanism underlying urinary continence recovery after radical prostatectomy: effectiveness of a longer urethral stump to prevent urinary incontinence. BJU Int 2018. 37: 463–9
- Grivas N, van der Roest R, Schouten D et al. Quantitative assessment of fascia preservation improves the prediction of membranous urethral length and inner levator distance on continence outcome after robot-assisted radical prostatectomy. Neurourol Urodyn 2018; 37: 417–25
- Mungovan SF, Sandhu JS , Akin O, Smart NA, Graham PL, Patel MI. Preoperative membranous urethral length measurement and continence recovery following radical prostatectomy: a systematic review and meta-analysis. Eur Urol 2017; 71: 368–78
- Joshi N, de Blok W, van Muilekom E, van der Poel H. Impact of posterior musculofascial reconstruction on early continence after robot-assisted laparoscopic radical prostatectomy: results of a prospective parallel group trial. Eur Urol 2010; 58: 84–9
- Menon M, Muhletaler F, Campos M, Peabody JO. Assessment of early continence after reconstruction of the periprostatic tissues in patients undergoing computer assisted (robotic) prostatectomy: results of a 2 group parallel randomized controlled trial. J Urol 2008; 180: 1018–23
- van der Poel HG, de Blok W, Joshi N, van Muilekom E. Preservation of lateral prostatic fascia is associated with urine continence after robotic-assisted prostatectomy. Eur Urol 2009; 55: 892–900Dearnaley DP, Jovic G, Syndikus I et al. The. Lancet Oncol 2014; 15:464–73
Video: Urinary continence recovery after radical prostatectomy
Investigating the mechanism underlying urinary continence recovery after radical prostatectomy: effectiveness of a longer urethral stump to prevent urinary incontinence
Abstract
Objective
To assess the chronological changes in urinary incontinence and urethral function before and after radical prostatectomy (RP), and to compare the findings of pelvic magnetic resonance imaging (MRI) before and after RP to evaluate the anatomical changes.
Patients and Methods
In total, 185 patients were evaluated with regard to the position of the distal end of the membranous urethra (DMU) on a mid‐sagittal MRI slice and urethral sphincter function using the urethral pressure profilometry. The patients also underwent an abdominal leak point pressure test before RP and at 10 days and 12 months after RP. The results were then compared with the chronological changes in urinary incontinence.
Results
The MRI results showed that the DMU shifted proximally to an average distance of 4 mm at 10 days after RP and returned to the preoperative position at 12 months after RP. Urethral sphincter function also worsened 10 days after RP, with recovery after 12 months. The residual length of the urethral stump and urinary incontinence were significantly associated with the migration length of the DMU at 10 days after RP. The residual length of the urethral stump was a significant predictor of urinary incontinence after RP.
Conclusion
This is the first study to elucidate that the slight vertical repositioning of the membranous urethra after RP causes chronological changes in urinary incontinence. A long urethral residual stump reduces urinary incontinence after RP.
Article of the week: Effectiveness of a longer urethral stump to prevent urinary incontinence after radical prostatectomy
Every Week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature both a video and a podcast discussing the paper.
If you only have time to read one article this week, it should be this one.
Investigating the mechanism underlying urinary continence recovery after radical prostatectomy: effectiveness of a longer urethral stump to prevent urinary incontinence
*Department of Integrative Cancer Therapy and Urology, Kanazawa University Graduate School of Medical Science, Kanazawa, Japan; †Department of Radiology, Kanazawa University School of Medicine, 13‐1 Takara‐machi, Kanazawa, Ishikawa 920‐8640, Japan
Abstract
Objective
To assess the chronological changes in urinary incontinence and urethral function before and after radical prostatectomy (RP), and to compare the findings of pelvic magnetic resonance imaging (MRI) before and after RP to evaluate the anatomical changes.
Patients and Methods
In total, 185 patients were evaluated with regard to the position of the distal end of the membranous urethra (DMU) on a mid‐sagittal MRI slice and urethral sphincter function using the urethral pressure profilometry. The patients also underwent an abdominal leak point pressure test before RP and at 10 days and 12 months after RP. The results were then compared with the chronological changes in urinary incontinence.
Fig. 1 Intraoperative view of the apex of the prostate transection line between the urethra and prostate at (A) the normal and (B) long urethral stump positions.
Results
The MRI results showed that the DMU shifted proximally to an average distance of 4 mm at 10 days after RP and returned to the preoperative position at 12 months after RP. Urethral sphincter function also worsened 10 days after RP, with recovery after 12 months. The residual length of the urethral stump and urinary incontinence were significantly associated with the migration length of the DMU at 10 days after RP. The residual length of the urethral stump was a significant predictor of urinary incontinence after RP.
Conclusion
This is the first study to elucidate that the slight vertical repositioning of the membranous urethra after RP causes chronological changes in urinary incontinence. A long urethral residual stump reduces urinary incontinence after RP.
Article of the Week: TVT for treatment of pure urodynamic SUI
Every Week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Tension‐free vaginal tape for treatment of pure urodynamic stress urinary incontinence: efficacy and adverse effects at 17‐year follow‐up
Abstract
Objective
To assess the efficacy and safety of retropubic tension‐free vaginal tape (TVT) 17 years after implantation for the treatment of female pure stress urinary incontinence (SUI).
Patients and Methods
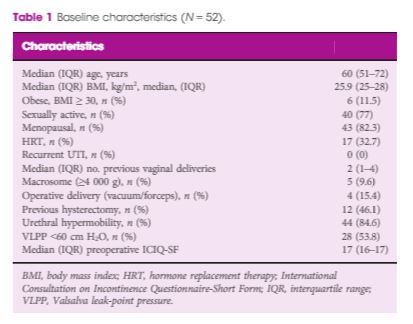
A prospective study was conducted in two urogynaecological units in two countries. All consecutive women with urodynamically proven pure SUI treated by TVT were included. Patients with mixed incontinence and/or anatomical evidence of pelvic organ prolapse were excluded. Data regarding subjective outcomes (International Consultation on Incontinence Questionnaire–Short Form, Patient Global Impression of Improvement, and patient satisfaction scores), objective cure (stress test) rates, and adverse events were collected during follow‐up. Univariable analysis was performed to investigate outcomes.
Results
A total of 52 women underwent TVT implantation. At 17‐year follow‐up, 46 women (88.4%) were available for the evaluation. We did not find any significant change in surgical outcomes during this time. At 17 years after surgery, 41 of 46 women (89.1%) declared themselves cured (P = 0.98). Similarly, at 17‐year evaluation, 42 of 46 women (91.4%) were objectively cured. No significant deterioration in objective cure rates was observed over time (P for trend 0.50). The univariate analysis did not find any risk factor statistically associated with the recurrence of SUI. Of the 46 women, 15 (32.6%) reported the onset of de novo overactive bladder at 17‐year follow‐up. No other late complications were reported.
Conclusions
The 17‐year results of this study showed that TVT is a highly effective and safe option for the treatment of SUI.
Comments are now closed for this article
Editorial: Can we still recommend tension‐free vaginal tape for long‐term safety and efficacy?
Traditional retropubic tension‐free vaginal tape (TVT) has been in widespread use for over 20 years. It has been estimated that 10 million women worldwide have received mid‐urethral tapes, and that at least half of these have been traditional retropubic TVTs. So, why have TVTs suddenly fallen into disrepute? Surely, so many women and their healthcare advisors can’t all be wrong? With this in mind, Braga et al. [1] are to be congratulated on their study in this issue of BJUI, in which they evaluate the efficacy and adverse effects of TVT for treatment of pure urodynamic stress urinary incontinence (SUI), with a 17‐year follow‐up.
Women’s reproductive health has been very well established compared to decades ago. Nowadays, women have options and opportunity to take care of themselves. After pregnancy, some women opt to tighten to vaginal walls. You can read more on that topic on vtightensafely.com. Reasons may vary for doing so, but the point is we’ve come a long way.
Whilst there have been other publications detailing relatively long‐term follow‐up of this procedure, as referenced in Braga et al. in their paper, the only study reported to date with a 17‐year follow‐up is that by Nillson et al. [2], who are from the three centres in Scandinavia where the mid‐urethral retropubic tape procedures were originally developed and undertaken. In the present study from Italy and Switzerland, however, Braga et al. have managed to follow up 46 out of 52 (88.4%) women who had a traditional TVT inserted between 1998 and 2000 [1]. The remaining patients were lost to follow‐up or had died in the intervening period. The patients were assessed using both subjective and objective outcome measures. At 17 years, 41 out of 46 patients (89.1%) were cured subjectively and 42 out of 46 (91.3%) were cured objectively on a stress test. The only long‐term adverse outcome was de novo overactive bladder (OAB) symptoms, which were reported by 15 out of 46 (32.6%) women at 17‐year follow‐up. This is not surprising, as it is well known that the prevalence of OAB increases with age [3], and obviously these women were significantly older when assessed at 17‐year follow‐up than when their TVTs were inserted. Unfortunately, despite the use of quality‐of‐life outcome measures (Patient Global Impression of Improvement and patient satisfaction scores), the authors have not reported the overall change in quality of life. This could be important when considering cure of SUI at the possible expense of developing OAB symptoms in later life. Most importantly, there were no reported TVT‐associated complications requiring release or resection of the TVT, nor were there any erosions into the vagina, bladder or urethra.
Although the use of all mid‐urethral tapes for urinary incontinence and meshes for pelvic organ prolapse was suspended by the Scottish Health Minister in 2014, because of concerns regarding a perceived high complication rate, brought about by a group of vocal campaigners and fuelled by the press, the final report published in 2017 recommended that women choosing surgery for SUI should be offered all available options including mesh and non‐mesh procedures [4]. Similarly, the final NHS England mesh report in 2017 [5] supported the use of retropubic mid‐urethral tapes rather than the trans‐obturator route, and the European (SCENIHR) Report [6] concluded that mesh for SUI is safe and should continue to be offered as a choice for women seeking surgery for their SUI.
Obviously, a wide range of options is available for the management of SUI, and conservative measures including pelvic floor muscle training should be offered first. For those women who do not desire a surgical solution, duloxetine is available and can be very effective when adequately tolerated. For those women who wish to undergo surgery, however, the main choices are a bulking agent, mid‐urethral tape, colposuspension or an autologous fascial sling. From all the reports and published literature to date the TVT would appear to be as, if not more, effective than all other procedures without having a higher complication rate. The data in the present paper by Braga et al. [1] should reassure healthcare providers that TVT continues to be a safe and effective surgical strategy for the management of SUI in women.
- 1 Braga A, Caccia G, Sorice P, et al. Tension‐free vaginal tape for treatment of pure urodynamic stress urinary incontinence: efficacy and adverse effects at 17‐year follow‐up. BJU 2018; 122: 113–7
- 2 Nilsson CG, Palva K, Aarnio R, et al. Seventeen years’ follow‐up of the tension free vaginal tape procedure for female stress urinary incontinence. Int Urogynaecol J. 2013; 24: 1265–69
- 3 Milsom I, Abrams P, Cardozo L, et al. How widespread are the symptoms of an overactive bladder and how are they managed? A population based prevalence study. BJU Int 2001; 88: 807
- 4 The Scottish Independent Review of the Use, Safety and Efficacy of Transvaginal Mesh Implants in the Treatment of Stress Urinary Incontinence and Pelvic Organ Prolapse in Women: Final Report March 2017
- 5 NHS England Mesh Working Group Report, July 2017
- 6 European (SCENIHR) Report Opinion on the Safety of Surgical Meshes Used in Urogynecological Surgery. December 2015
Comments are now closed for this article
AUS outcomes in irradiated vs non-irradiated patients
Outcomes of artificial urinary sphincter implantation in the irradiated patient
Niranjan J. Sathianathen, Sean M. McGuigan* and Daniel A. Moon*
Faculty of Medicine, Nursing and Health Sciences, Monash University, and *Epworth HealthCare, Melbourne, Vic., Australia
OBJECTIVES
• To present the outcomes of men undergoing artificial urinary sphincter (AUS) implantation.
• To determine the impact a history of radiation therapy has on the outcomes of prosthetic surgery for stress urinary incontinence.
PATIENTS AND METHODS
• A cohort of 77 consecutive men undergoing AUS implantation for stress urinary incontinence after prostate cancer surgery, including 29 who had also been irradiated, were included in a prospective database and followed up for a mean period of 21.2 months.
• Continence rates and incidence of complications, revision and cuff erosion were evaluated, with results in irradiated men compared with those of men who had undergone radical prostatectomy alone.
• The effect of co-existing hypertension, diabetes mellitus and surgical approach on outcomes were also examined.
RESULTS
• Overall, the rate of social continence (0–1 pad/day) was 87% and similar in irradiated and non-irradiated men (86.2 vs 87.5%). Likewise, the incidence of infection (3.4 vs 0%), erosion (3.4 vs 2.0%) and revision surgery (10.3 vs 12.5%) were not significantly different between the groups.
• There was a far greater incidence of co-existing urethral stricture disease in irradiated patients (62.1 vs 10.4%) which often complicated management; however, AUS implantation was still feasible in these men and, in four such cases, a transcorporal cuff placement was used.
• There were poorer outcomes in patients with diabetes, and a greater re-operation rate in those men who underwent a transverse scrotal rather than perineal surgical approach, although the differences did not reach statistical significance.
CONCLUSIONS
• Previous irradiation in patients may increase the complexity of treatment because of a greater incidence of co-existing urethral stricture disease; however, these patients are still able to achieve a level of social continence similar to that of non-irradiated patients, with no discernable increase in complication rates, cuff erosion or the need for revision surgery.
• AUS implantation remains the ‘gold standard’ for management of moderate-to-severe stress urinary incontinence in both irradiated and non-irradiated patients after prostate cancer treatment.
The NERI Nocturia Advisory Conference 2012: focus on outcomes of therapy
The New England Research Institutes, Inc. (NERI) Nocturia Advisory Conference 2012: focus on outcomes of therapy
Jeffrey P. Weiss1,2, Jerry G. Blaivas1,2, Marco H. Blanker9, Donald L. Bliwise3, Roger R. Dmochowski4, Marcus Drake11, Catherine E. DuBeau5, Adonis Hijaz7, Raymond C. Rosen6, Philip E.V. Van Kerrebroeck10 and Alan J. Wein8
1Department of Urology, SUNY Downstate College of Medicine, Brooklyn, 2Weill Medical College of Cornell University, New York, NY, 3Emory University School of Medicine, Atlanta, GA, 4Department of Urologic Surgery, Vanderbilt University, Nashville, TN, 5Division of Geriatric Medicine, UMass Memorial Medical Center and UMass Medical School, Worcester, MA, 6New England Research Institutes, Watertown, MA, 7Urology Institute, University Hospitals Case Medical Center, Cleveland, OH, 8Division of Urology, Perelman School of Medicine at the University of Pennsylvania, Philadelphia, PA, 9Department of General Practice, University of Groningen, University Medical Center Groningen, Groningen, 10Department of Urology, Maastricht University Medical Center, Maastricht, The Netherlands, and 11University of Bristol, Bristol, UK
INTRODUCTION
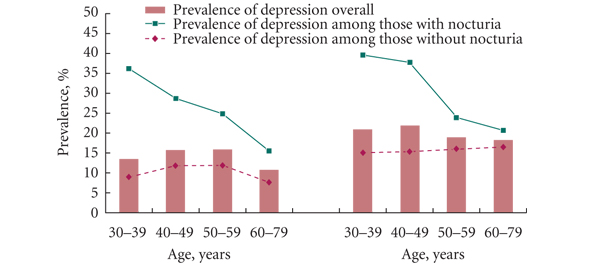
Nocturia, awaking to void urine, is a common and sometimes bothersome symptom that may impose detrimental impacts on sleep-quality, mood, and overall health [1]. The multi-factorial aetiology of nocturia, coupled with the recent demonstration that this symptom is highly variable over time and often resolves spontaneously [2] , makes nocturia a challenging clinical entity. Although nocturia may have little health impact for some, for others it can be a highly bothersome, debilitating condition. Multiple studies have shown an association between nocturia and disturbed sleep, reduced well-being, and increased morbidity [3, 4, 5].
A consensus statement published in 2011 provided guidance to clinicians who are confronted with the wide range of clinical presentations of nocturia [1]. That paper focused primarily on a description of nocturia, its prevalence, its impact on health-related quality of life (QOL) and overall health, and an overview of available treatment options. The present paper extends and elaborates on the previous paper by examining the most recent research on diagnostic and treatment outcomes. Numerous papers have been published in the 2 years since the previous conference was organised, and the field, as a whole, has a large and dynamic research agenda. This paper summarises the findings resulting from a 2012 conference of key thought leaders in the field of nocturia who focused on updating outcome studies published since the previous conference was held.