Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial written by a prominent member of the urological community and a video prepared by the authors. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Jonathan B. Bloom*, Amir H. Lebastchi*, Samuel A. Gold*, Graham R. Hale*, Thomas Sanford*†, Sherif Mehralivand*†‡, Michael Ahdoot*, Kareem N. Rayn*, Marcin Czarniecki†, Clayton Smith†, Vladimir Valera*, Bradford J. Wood§, Maria J. Merino¶, Peter L. Choyke†, Howard L. Parnes**, Baris Turkbey† and Peter A. Pinto*§
*Urologic Oncology Branch, †Molecular Imaging Program, NCI, NIH, Bethesda, MD, USA, ‡Department of Urology and Pediatric Urology, University Medical Center Mainz, Mainz, Germany, §Center for Interventional Oncology, ¶Laboratory of Pathology, and **Division of Cancer Prevention, NCI, NIH, Bethesda, MD, USA
Abstract
Objectives
To determine the rate of Gleason Grade Group (GGG) upgrading in African‐American (AA) men with a prior diagnosis of low‐grade prostate cancer (GGG 1 or GGG 2) on 12‐core systematic biopsy (SB) after multiparametric magnetic resonance imaging (mpMRI) and fusion biopsy (FB); and whether AA men who continued active surveillance (AS) after mpMRI and FB fared differently than a predominantly Caucasian (non‐AA) population.
Patients and methods
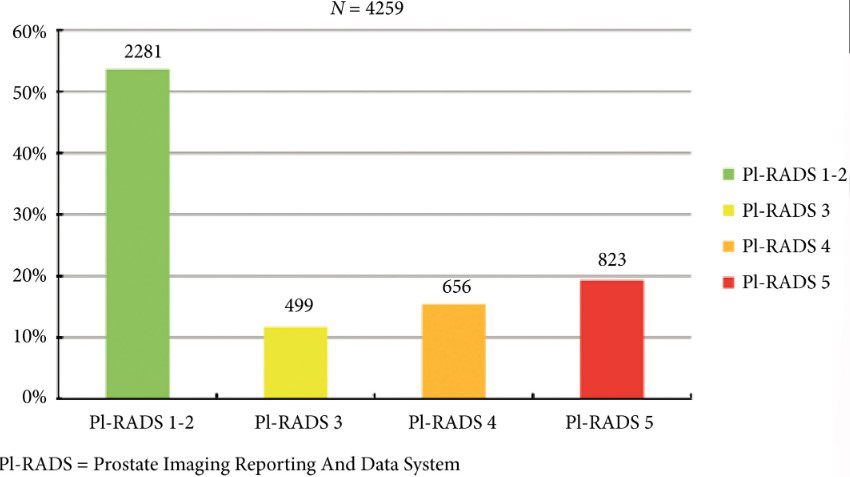
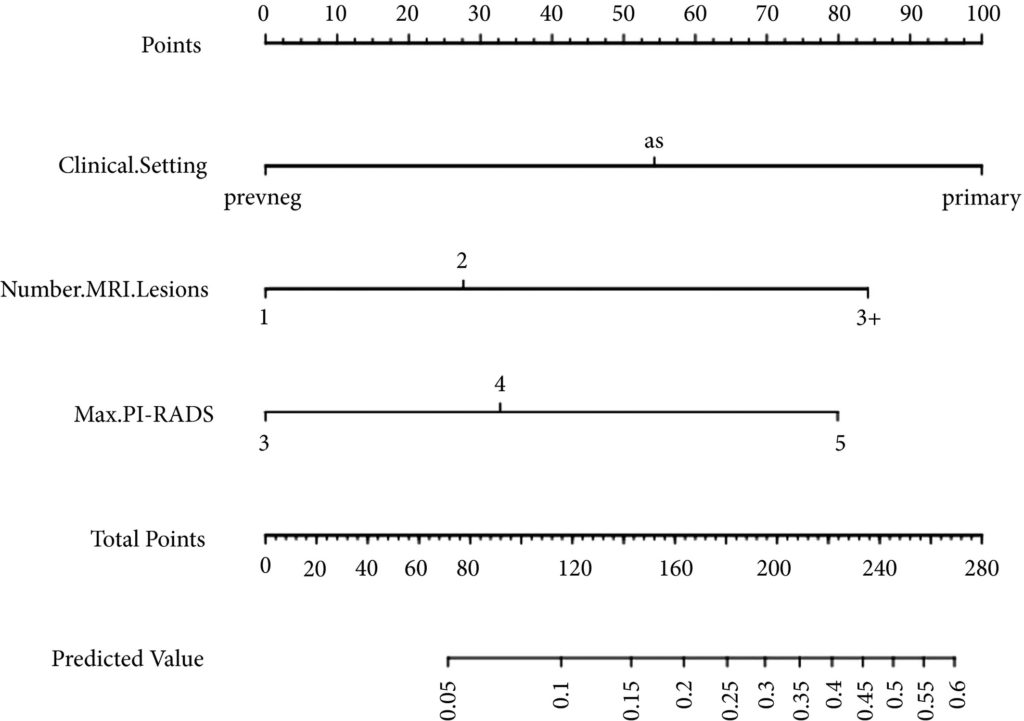
A database of men who had undergone mpMRI and FB was queried to determine rates of upgrading by FB amongst men deemed to be AS candidates based on SB prior to referral. After FB, Kaplan–Meier curves were generated for AA men and non‐AA men who then elected AS. The time to GGG upgrading and time continuing AS were compared using the log‐rank test.
Results
AA men referred with GGG 1 disease on previous SB were upgraded to GGG ≥3 by FB more often than non‐AA men, 22.2% vs 12.7% (P = 0.01). A total of 32 AA men and 258 non‐AA men then continued AS, with a median (interquartile range) follow‐up of 39.19 (24.24–56.41) months. The median time to progression was 59.7 and 60.5 months, respectively (P = 0.26). The median time continuing AS was 61.9 months and not reached, respectively (P = 0.80).
Conclusions
AA men were more likely to be upgraded from GGG 1 on SB to GGG ≥3 on initial FB; however, AA and non‐AA men on AS subsequently progressed at similar rates following mpMRI and FB. A greater tendency for SB to underestimate tumour grade in AA men may explain prior studies that have shown AA men to be at higher risk of progression during AS.