Posts
Article of the week: The impact on oncological outcomes after RP for PCa of converting soft tissue margins at the apex and bladder neck from tumour‐positive to ‐negative
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial written by a prominent member of the urological community and the authors have also kindly produced a video describing their work. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
The impact on oncological outcomes after radical prostatectomy for prostate cancer of converting soft tissue margins at the apex and bladder neck from tumour‐positive to ‐negative
Abstract
Objectives
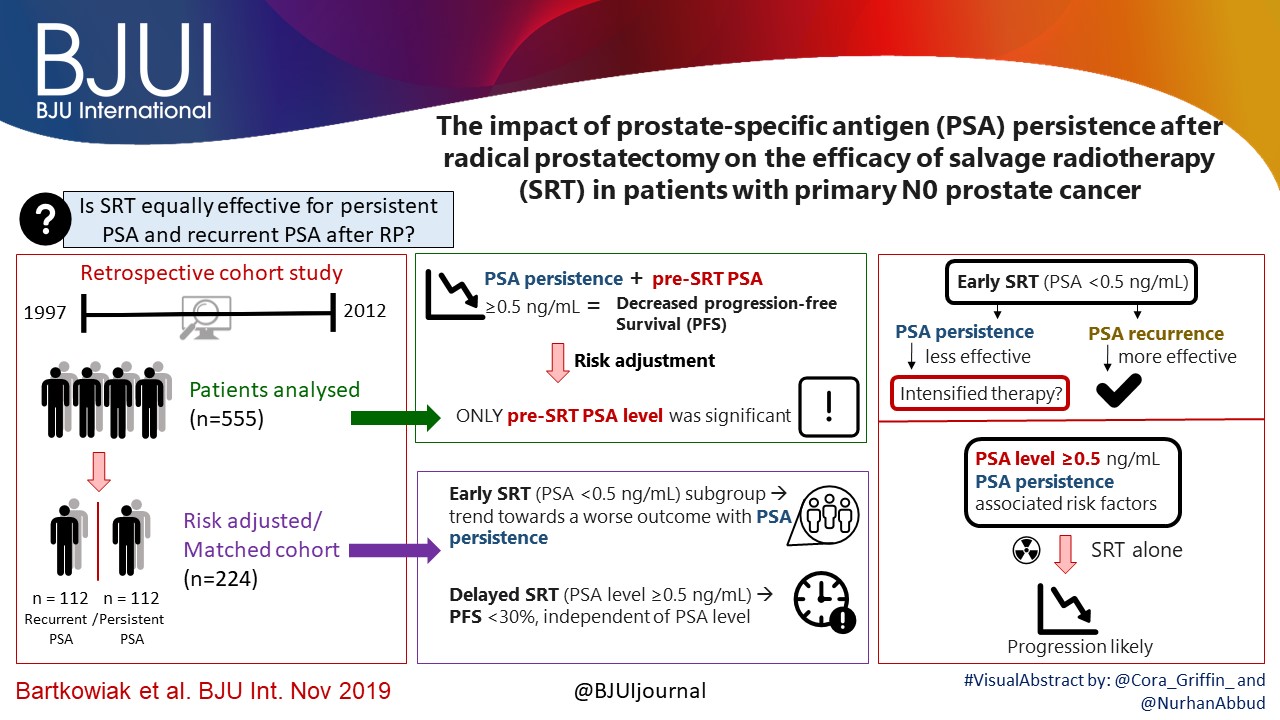
To assess the impact of conversion from histologically positive to negative soft tissue margins at the apex and bladder neck on biochemical recurrence‐free survival (BCRFS) and distant metastasis‐free survival (DMFS) after radical prostatectomy (RP) for prostate cancer.
Materials and Methods
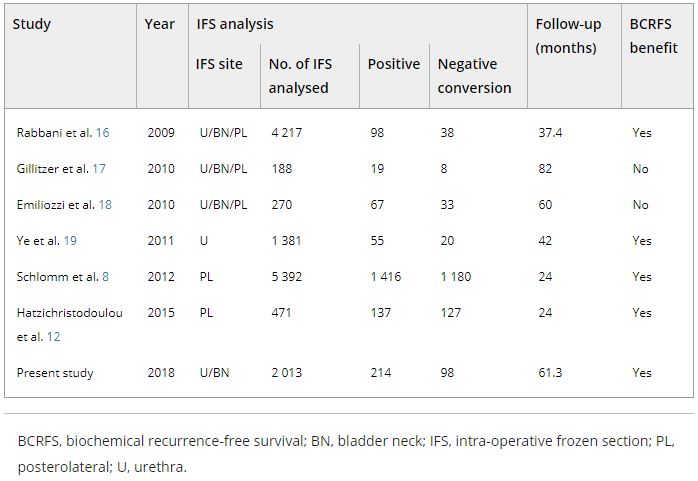
The records of 2 013 patients who underwent RP and intra‐operative frozen section (IFS) analysis between July 2007 and June 2016 were reviewed. IFS analysis of the urethra and bladder neck was performed, and if malignant or atypical cells remained, further resection with the aim of achieving histological negativity was carried out. Patients were divided into three groups according to the findings: those with a negative surgical margin (NSM), a positive surgical margin converted to negative (NCSM) and a persistent positive surgical margin (PSM).
Table 4. Impact of converting margins from tumour‐positive to ‐negative on biochemical recurrence
Results
Among the 2 013 patients, rates of NSMs, NCSMs and PSMs were 75.1%, 4.9%, and 20.0%, respectively. The 5‐year BCRFS rates of patients with NSMs, NCSMs and PSMs were 89.6%, 85.1% and 57.1%, respectively (P < 0.001). In both pathological (p)T2 and pT3 cancers, the 5‐year BCRFS rate for patients with NCSMs was similar to that for patients with NSMs, and higher than for patients with PSMs. The 7‐year DMFS rates of patients with NSMs, NCSMs and PSMs were 97.8%, 99.1% and 89.4%, respectively (P < 0.001). Among patients with pT3 cancers, the 7‐year DMFS rate was significantly higher in the NCSM group than in the PSM group (98.0% vs 86.7%; P = 0.023), but not among those with pT2 cancers (100% vs 96.9%; P = 0.616). The 5‐year BCRFS rate for the NCSM group was not significantly different from that of the NSM group among the patients with low‐ (96.3% vs 95.8%) and intermediate‐risk disease (91.1% vs 82.8%), but was lower than that of the NSM group among patients in the high‐risk group (73.2% vs 54.7%).
Conclusions
Conversion of the soft tissue margin at the prostate apex and bladder neck from histologically positive to negative improved the BCRFS and DMFS after RP for prostate cancer; however, the benefit of conversion was not apparent in patients in the high‐risk group.
Video: The impact on oncological outcomes after RP for PCa of converting soft tissue margins at the apex and bladder neck from tumour‐positive to ‐negative
The impact on oncological outcomes after radical prostatectomy for prostate cancer of converting soft tissue margins at the apex and bladder neck from tumour‐positive to ‐negative
Abstract
Objectives
To assess the impact of conversion from histologically positive to negative soft tissue margins at the apex and bladder neck on biochemical recurrence‐free survival (BCRFS) and distant metastasis‐free survival (DMFS) after radical prostatectomy (RP) for prostate cancer.
Materials and Methods
The records of 2 013 patients who underwent RP and intra‐operative frozen section (IFS) analysis between July 2007 and June 2016 were reviewed. IFS analysis of the urethra and bladder neck was performed, and if malignant or atypical cells remained, further resection with the aim of achieving histological negativity was carried out. Patients were divided into three groups according to the findings: those with a negative surgical margin (NSM), a positive surgical margin converted to negative (NCSM) and a persistent positive surgical margin (PSM).
Results
Among the 2 013 patients, rates of NSMs, NCSMs and PSMs were 75.1%, 4.9%, and 20.0%, respectively. The 5‐year BCRFS rates of patients with NSMs, NCSMs and PSMs were 89.6%, 85.1% and 57.1%, respectively (P < 0.001). In both pathological (p)T2 and pT3 cancers, the 5‐year BCRFS rate for patients with NCSMs was similar to that for patients with NSMs, and higher than for patients with PSMs. The 7‐year DMFS rates of patients with NSMs, NCSMs and PSMs were 97.8%, 99.1% and 89.4%, respectively (P < 0.001). Among patients with pT3 cancers, the 7‐year DMFS rate was significantly higher in the NCSM group than in the PSM group (98.0% vs 86.7%; P = 0.023), but not among those with pT2 cancers (100% vs 96.9%; P = 0.616). The 5‐year BCRFS rate for the NCSM group was not significantly different from that of the NSM group among the patients with low‐ (96.3% vs 95.8%) and intermediate‐risk disease (91.1% vs 82.8%), but was lower than that of the NSM group among patients in the high‐risk group (73.2% vs 54.7%).
Conclusions
Conversion of the soft tissue margin at the prostate apex and bladder neck from histologically positive to negative improved the BCRFS and DMFS after RP for prostate cancer; however, the benefit of conversion was not apparent in patients in the high‐risk group.
Re: Millin’s prostatectomy in the era of ‘Getting It Right First Time’ and Montgomery: exploring variation in clinical practice and consent
Letter to the Editor
Millin’s prostatectomy in the era of ‘Get it Right First Time’ and Montgomery: exploring variation in clinical practice and consent.
We read with interest the comment in last months BJUI where it was suggested that the Millin retropubic simple prostatectomy for BPH should be confined to history in part because of the Montgomery ruling and the GIRFT programme [1]. GIRFT was designed to identify variations and raise standards of care. The urology report has since been published (it was not available when the original article was written) and Simon Harrison and his team should be congratulated for providing an excellent review of the current state of urology in the UK and identifying recommendations to improve patient care [2]. As surgeons we are acutely aware how the Montgomery ruling has shifted the test for appropriate consent from the “Bolam principle” to a patient orientated process. It is no longer for us to deem what information is relevant to inform the patient and all risks/benefits/alternatives must be outlined. We should all use a detailed, patient-centred, longitudinal approach to consent supplemented with BAUS information leaflets and other resources.
Where we disagree with the authors is to suggest that both of these key events (GIRFT and Montgomery) can be interpreted as justification for not performing a highly effective operation with excellent outcomes. Terence Millin described the transcapsular retropubic simple prostatectomy in 1945 and it revolutionised the management of men with BPH. There are few other procedures that have survived since their inception over 70 years ago in the same form [3] and it remains an established treatment for large glands in European, British and American urological guidelines respectively. More recently the robotic platform has been utilised to perform the technique, although more frequently a transvesical approach is deployed. When performed by well-trained surgeons it remains a procedure that yields very high patient satisfaction and low complication rates. Whilst accepting the cost implications of the slight increased length of stay the authors have failed to discuss the hidden costs of consumables, increased theatre time and further treatments that may be required for the transurethral enucleation procedures.
HES data shows that Millin prostatectomy is not a commonly performed operation. This reflects the fact that massively enlarged prostates are not as common as in the past, partly due to the widespread use of medical therapy and earlier referrals. However, the management of the extreme end of the enlarged benign prostate will always be challenging and we feel that there remains a need to have surgeons with the necessary skills to perform this procedure in the appropriately selected and consented patient. The largest adenoma enucleated by the authors is 980cc (GW) and we would suggest that this would represent a challenge for any transurethral approach. Indeed, the previous Editor of this journal commented in 2008 “some have said that the era of the Millin prostatectomy is over. I very much disagree with this and would not like to see the demise of such a satisfying surgical procedure, with excellent outcome for the patient” [4].
Andrew Chetwood1, Pravin Menezes2, Charles Coker3, Graham Watson4
1Frimley Health NHS Foundation Trust
2Kingston Hospital NHS Trust
3Brighton and Sussex University Hospitals NHS Trust
4East Sussex Hospitals NHS trust
References
- Millin’s prostatectomy in the era of ‘getting it Right First Time’ and Montgomery: exploring variation in clinical practice and consent. Malthouse T, Mistry K, Agrawal S. BJU Int 2018;122:171-172
- gettingitrightfirsttime.co.uk
- Retropubic prostatectomy; a new extravesical technique; report of 20 cases. Millin Lancet. 1945 Dec 1;2(6380):693-6.
- Surgery Illustrated – Millin Retropubic Prostatectomy. Fitzpatrick J, BJU Int 2008;102:906-916
Reply by the authors
We wholeheartedly agree that the Millin’s is indeed a ‘satisfying surgical procedure, with excellent outcomes for the patient’ and it is not a procedure we would voluntarily relinquish. However as surgeons we should bear in mind the fundamental principles of ‘primum non nocere’ and need to put patient safety above our own wishes to perform a specific operation. There have been several technological advances since 2008, with HOLEP at the forefront of BPE surgery for large volume glands showing safer and equally effective outcomes. Indeed Terence Millen was a proponent of transurethral techniques developing his own Millin’s resectoscope, with the retropubic approach only evolving due to a lack of equipment after the world war. He may well have been the first to innovate.
Our article was designed to stimulate a debate around consent, safety, and cost effectiveness in our whole practice. However the principles outlined within GIRFT ideology and the current medicolegal world we live in, remain. Consent for a Millin’s is clearly an issue with the need to specifically discuss (and document) alternatives including HOLEP, with evidence clearly showing improved safety, lower morbidity and length of stay. Additionally the majority of NHS trusts, have a centre within their region delivering this service and as such not offering HOLEP would not justify performing a Millin’s. Whilst we accept that newer minimally invasive techniques (robotic/laparoscopic with similar safety profiles) also exist and could be retained for the larger glands, we suspect the majority of open retropubic prostatectomies are not for 980cc volume prostates.
Finally, we would argue the fact that HES data shows the Millin’s to be a low volume procedure suggesting many have already changed practice. When considering costs towards consumables, these are incorporated and not in addition to tariffs paid to organisations. As tax paying members of the public and as clinicians we have a responsibility to use our funding and resources wisely. We believe that the literature would benefit from a modern-day case series to better inform this debate. Perhaps we need to define a volumetric cut off above which a retropubic or minimally invasive technique would be justifiable or cost effective?
Sachin Agrawal and Theo Malthouse
Ashford & St Peters NHS Foundation Trust
Article of the Week: Comparing LRP and RARP to ORP to treat PCa
Every Week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Laparoscopic and robot‐assisted vs open radical prostatectomy for the treatment of localized prostate cancer: a Cochrane systematic review
Abstract
Objective
To determine the effects of laparoscopic radical prostatectomy (LRP), or robot‐assisted radical prostatectomy (RARP) compared with open radical prostatectomy (ORP) in men with localized prostate cancer.
Materials and Methods
We performed a comprehensive search using multiple databases (CENTRAL, MEDLINE, EMBASE) and abstract proceedings, with no restrictions on the language of publication or publication status, up until 9 June 2017. We included all randomized or pseudo‐randomized controlled trials that directly compared LRP and RARP with ORP. Two review authors independently examined full‐text reports, identified relevant studies, assessed the eligibility of studies for inclusion, extracted data and assessed risk of bias. We performed statistical analyses using a random‐effects model and assessed the quality of the evidence according to Grading of Recommendations Assessment, Development and Evaluation (GRADE). The primary outcomes were prostate cancer‐specific survival, urinary quality of life and sexual quality of life. Secondary outcomes were biochemical recurrence‐free survival, overall survival, overall surgical complications, serious postoperative surgical complications, postoperative pain, hospital stay and blood transfusions.
Results
We included two unique studies in a total of 446 randomized participants with clinically localized prostate cancer. All available outcome data were short‐term (up to 3 months). We found no study that addressed the outcome of prostate cancer‐specific survival. Based on one trial, RARP probably results in little to no difference in urinary quality of life (mean difference [MD] −1.30, 95% confidence interval [CI] −4.65 to 2.05; moderate quality of evidence) and sexual quality of life (MD 3.90, 95% CI: −1.84 to 9.64; moderate quality of evidence). No study addressed the outcomes of biochemical recurrence‐free survival or overall survival. Based on one trial, RARP may result in little to no difference in overall surgical complications (risk ratio [RR] 0.41, 95% CI: 0.16−1.04; low quality of evidence) or serious postoperative complications (RR 0.16, 95% CI: 0.02–1.32; low quality of evidence). Based on two studies, LRP or RARP may result in a small, possibly unimportant improvement in postoperative pain at 1 day (MD −1.05, 95% CI: −1.42 to −0.68; low quality of evidence) and up to 1 week (MD −0.78, 95% CI: −1.40 to −0.17; low quality of evidence). Based on one study, RARP probably results in little to no difference in postoperative pain at 12 weeks (MD 0.01, 95% CI: −0.32 to 0.34; moderate quality of evidence). Based on one study, RARP probably reduces the length of hospital stay (MD −1.72, 95% CI: −2.19 to −1.25; moderate quality of evidence). Based on two studies, LRP or RARP may reduce the frequency of blood transfusions (RR 0.24, 95% CI: 0.12–0.46; low quality of evidence). Assuming a baseline risk for a blood transfusion to be 8.9%, LRP or RARP would result in 68 fewer blood transfusions per 1,000 men (95% CI: 78–48 fewer).
Conclusions
There is no evidence to inform the comparative effectiveness of LRP or RARP compared with ORP for oncological outcomes. Urinary and sexual quality of life appear similar. Overall and serious postoperative complication rates appear similar. The difference in postoperative pain may be minimal. Men undergoing LRP or RARP may have a shorter hospital stay and receive fewer blood transfusions.
Editorial: RARP and a Parachute
Radical prostatectomy is probably the most scrutinized, debated and re‐invented procedure in the field of urology. This is with good reason. Dr Hugh Hampton Young gave the first formal account of a radical treatment for prostate cancer in 1905. It was a procedure performed perineally with the prime intention of total cancer extirpation. The oncological results were tremendous given the nascency of the procedure. Functional outcomes, however, were less so, with only ~25% of the patients achieving urinary continence and almost none achieving potency 1. Seminal studies undertaken by Drs Patrick C. Walsh and Pieter J. Donker in the 1980s led to the next major advance in technique: nerve‐sparing. It lead to dramatic improvements in sexual and urinary function preservation, with urinary continence achieved in upwards of 90% and potency in upwards of 60% of patients 2, 3. Nerve‐sparing retropubic radical prostatectomy was rapidly adopted by urologists across the world. No randomized trial was conducted as the operation ‘made sense’, and it would have been unethical to offer patients an alternative, inferior operation. Retropubic radical prostatectomy, however, remained a morbid operation that was difficult to master; 1 200 mL blood loss and 20% incontinence, 15% stricture and 60–90% erectile dysfunction rates were the norm. Robot‐assisted surgery changed much of this. This surgery was perfected and popularized by Dr Mani Menon and his team at the Henry Ford Hospital. Blood loss dropped to ~100 mL, and incontinence and stricture rates today are ~1–5% with potency rates between 70% and 80% 4.
In the systematic review by Ilic et al. 5 trials that compared open with minimally invasive radical prostatectomy were evaluated. The authors are commended for combing through vast quantities of data to arrive at the final sample of two clinical trials (one laparoscopic, one robot‐assisted). The authors found no data on oncological endpoints. With respect to functional outcomes, the data reported in their systematic review are essentially from the recent Yaxley trial. It is true that randomized controlled trials form the backbone of medical progress, but they must be interpreted with care. The Yaxley trial has been criticized for comparing surgeons of vastly varying surgical expertise (1 500‐case experience for open prostatectomies, 200‐case experience for robot‐assisted prostatectomies), having a small sample size (~150 patients in each arm) and having a limited follow‐up (3 months). In line with this, Dr Gordon Smith has eloquently argued about the judicious use of randomized trials in evidence‐based medicine in his classic paper on parachutes and gravitational challenge 6. It is our sincere belief that robot‐assisted radical prostatectomy is a procedure in the service of the patients, and we believe that anyone who has performed both an open radical prostatectomy and a robot‐assisted radical prostatectomy would agree. Operating deep in the pelvis and being able to visualize the anatomy up‐close with robotic assistance ‘makes sense’, much like the anatomical radical prostatectomy did in the 1980s 2, 3.
‘If it ain’t broke, don’t fix it’, the old saying goes. In case of radical prostatectomy, the converse has been true, for the most part. The procedure is still not perfect, and nuances need to be worked out. Nonetheless, over the last century, radicalprogress has been made in the surgery for prostate; the two issues that now remain to be solved are: improving potency and improving cost‐effectiveness. With the potential arrival of competing robotic systems and improvements in technology, the costs associated with robotic surgery may become less of an issue in the future. With regard to potency, focal therapies, whether surgical or otherwise, hold promise.
- 1 Young HH. The cure of cancer of the prostate by radical perineal prostatectomy (prostato‐seminal Vesiculectomy): History, Literature and Statistics of Young’s Operation1. J Urol 1945; 53: 188–252
- 2 Walsh PC, Donker PJ. Impotence following radical prostatectomy: insight into etiology and prevention. J Urol 1982; 128: 492–7
- 3 Walsh PC, Lepor H, Eggleston JC. Radical prostatectomy with preservation of sexual function: anatomical and pathological considerations. Prostate 1983; 4: 473–85
- 4 Menon M, Dalela D, Jamil M et al. Functional recovery, oncologic outcomes and postoperative complications after robot‐assisted radical prostatectomy: an evidence‐based analysis comparing the Retzius sparing and standard approaches. J Urol 2018; 199: 1210–7
- 5 Ilic D, Evans SM, Allan CA, Jung JH, Murphy D, Frydenberg M. Laparoscopic and robot‐assisted vs open radical prostatectomy for the treatment of localized prostate cancer: a Cochrane systematic review. BJU Int 2018; 121: 845–53
- 6 Smith GC, Pell JP. Parachute use to prevent death and major trauma related to gravitational challenge: systematic review of randomised controlled trials. BMJ 2003; 20: 1459–61
Residents’ Podcast: Pelvic Drain Placement After Robot-Assisted Radical Prostatectomy
Department of Urology, Dalhousie University, Halifax, NS, Canada
Abstract
Objective
To determine if eliminating the prophylactic placement of a pelvic drain (PD) after robot-assisted radical prostatectomy (RARP) affects the incidence of early (90-day) postoperative adverse events.
Patients and Methods
In this parallel-group, blinded, non-inferiority trial, we randomised patients planning to undergo RARP to one of two arms: no drain placement (ND) or PD placement. Patients with demonstrable intraoperative leakage upon bladder irrigation were excluded. Randomisation sequence was determined a priori using a computer algorithm, and included a stratified design with respect to low vs intermediate/high D’Amico risk classifications. Surgeons remained blinded to the randomisation arm until final eligibility was verified at the end of the RARP. The primary endpoint was overall incidence of 90-day complications which, based on our standard treatment using PD retrospectively, was estimated at 13%. The non-inferiority margin was set at 10%, and the planned sample size was 312. An interim analysis was planned and conducted when one-third of the planned accrual and follow-up was completed, to rule out futility if the delta margin was in excess of 0.1389.
Results
From 2012 to 2016, 189 patients were accrued to the study, with 92 patients allocated to the ND group and 97 to the PD group. Due to lower than expected accrual rates, accrual to the study was halted by regulatory entities, and we did not reach the intended accrual goal. The ND and PD groups were comparable for median PSA level (6.2 vs 5.8 ng/mL, P = 0.5), clinical stage (P = 0.8), D’Amico risk classification (P = 0.4), median lymph nodes dissected (17 vs 18, P = 0.2), and proportion of patients receiving an extended pelvic lymph node dissection (70.7% vs 79.4%, P = 0.3). Incidence of 90-day overall and major (Clavien–Dindo grade >III) complications in the ND group (17.4% and 5.4%, respectively) was not inferior to the PD group (26.8% and 5.2%, respectively; P < 0.001 and P = 0.007 for difference of proportions <10%, respectively). Symptomatic lymphocoele rates (2.2% in the ND group, 4.1% in the PD group) were comparable between the two arms (P = 0.7).
Conclusions
Incidence of adverse events in the ND group was not inferior to the group who received a PD. In properly selected patients, PD placement after RARP can be safely withheld without significant additional morbidity.
BJUI Podcasts now available on iTunes, subscribe here https://itunes.apple.com/gb/podcast/bju-international/id1309570262
Article of the Week: Chitosan membranes applied on the prostatic neurovascular bundles after nerve‐sparing robot‐assisted radical prostatectomy: a phase II study
Every Week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this month, it should be this one.
Chitosan membranes applied on the prostatic neurovascular bundles after nerve‐sparing robot‐assisted radical prostatectomy: a phase II study
Abstract
Objective
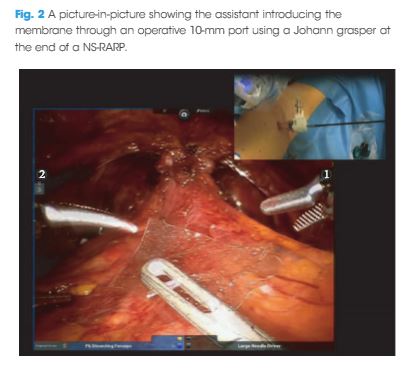
To evaluate the feasibility and the safety of applying chitosan membrane (ChiMe) on the neurovascular bundles (NVBs) after nerve‐sparing robot‐assisted radical prostatectomy (NS‐RARP). The secondary aim of the study was to report preliminary data and in particular potency recovery data.
Patients and Methods
This was a single‐centre, single‐arm prospective study, enrolling all patients with localised prostate cancer scheduled for RARP with five‐item version of the International Index of Erectile Function scores of >17, from July 2015 to September 2016. All patients underwent NS‐RARP with ChiMe applied on the NVBs. The demographics, perioperative, postoperative and complications data were evaluated. Potency recovery data were evaluated in particular and any sign/symptom of local allergy/intolerance to the ChiMe was recorded and evaluated.
Results
In all, 140 patients underwent NS‐RARP with ChiMe applied on the NVBs. Applying the ChiMe was easy in almost all the cases, and did not compromise the safety of the procedure. None of the patients reported signs of intolerance/allergy attributable to the ChiMe and potency recovery data were encouraging.
Conclusion
In our experience, ChiMe applied on the NVBs after NS‐RARP was feasible and safe, without compromising the duration, difficulty or complication rate of the ‘standard’ procedure. No patients had signs of intolerance/allergy attributable to the ChiMe and potency recovery data were encouraging. A comparative cohort would have added value to the study. The present paper was performed before Conformité Européene (CE)‐mark achievement.
Editorial: Nerve wrapping with biomaterials during radical prostatectomy to improve potency recovery
Radical prostatectomy is one of the standard treatment options for localized prostate cancer. The functional outcomes of radical prostatectomy are steadily improving along with better understanding of the surgical anatomy involved. Technological and technical advancements have helped improve continence outcomes significantly. High‐volume centres have consistently reported continence rates of >95% 1; however, potency recovery is the major limiting factor in achieving trifecta, even with full nerve‐sparing. Neuropraxia secondary to surgical dissection is one of the factors delaying potency recovery. We were the first to introduce the concept of protecting the neurovascular bundle using a wrap. In 2015, we first published our work on dehydrated human amnion‐chorion membrane (dHACM) nerve wrapping, a potential means of improving functional outcomes after radical prostatectomy 2.
Clinical applications of biomaterials are increasingly being explored. Their biological and physiochemical properties influence their role in peripheral nervous system regenerative therapy 3. Amniotic membrane graft has multiple growth factors including epidermal growth factor, vascular endothelial growth factor and anti‐inflammatory chemokines and cytokines including interleukin (IL)‐1, IL‐10 and IL‐1ra. In vitro and in vivo studies have reported that dHACM minimizes the surgical trauma‐induced inflammation and peri‐neural adhesions. These membranes are commercially available in various sizes for clinical use.
Porpiglia et al. 4 have reported their work on chitosan membrane application on the prostatic neurovascular bundle. Their phase II study is a step towards finding an ideal biomaterial favouring peripheral nerve healing. Chitosan is another potential biomaterial made of glucosamine and N‐acetyl glucosamine polymer which are natural components of mammalian tissues 5. Chitosan is hypoallergenic and only transiently stimulates the immune system and ultimately becomes bio‐tolerated and metabolized. It is not possible to develop specific antibodies against it because there are no proteins and lipids in its structure. Chitosan has inherent antimicrobial activity as its positive loads destabilize the membrane integrity of microorganisms. The inherent haemostatic and antimicrobial action of chitosan favour its application in wound healing. Chitosan has been extensively researched as a carrier molecule for biologically active particles and a scaffold in tissue engineering. Porpiglia et al. 4 have reported the safety and feasibility of its application for neurovascular bundle wrap during radical prostatectomy. In their non‐comparative study, they observed 96.4% continence and 68.6% potency recovery within 6 months. Comparative clinical trials are recommended to study its advantages in both partial and full nerve‐sparing settings. Membranes were manufactured from chitosan solution and sterilized for the purposes of the study. Pending approval by the regulators, study in other centres using chitosan membrane may be challenging.
The urological community has long been searching for ways to optimize functional outcomes after radical prostatectomy. Even for an ideal candidate with full nerve‐sparing, potency recovery is not assured. Several technical and technological modifications are being explored to address this concern. Bio-materials hold potential, and further exploration is warranted in the form of multicentre and randomized trials.
- 1 Patel VR, Abdul‐Muhsin HM, Schatloff O et al.Critical review of ‘pentafecta’ outcomes after robot‐assisted laparoscopic prostatectomy in high‐volume centres. BJU Int2011; 108: 1007–17
- 2 Patel VR, Samavedi S, Bates AS et al.Dehydrated Human Amnion/Chorion membrane allograft nerve wrap around the prostatic neurovascular bundle accelerates early return to continence and potency following robot‐assisted radical prostatectomy: propensity score‐matched analysis. Eur Urol2015; 67: 977–80
- 3 Dalamagkas K, Tsintou M, Seifalian A. Advances in peripheral nervous system regenerative therapeutic strategies: a biomaterials approach. Mater Sci Eng C Mater Biol Appl2016; 65: 425–32
- 4 Porpiglia F, Bertolo R, Fiori C, Manfredi M, De Cillis S, Geuna S. Chitosan membranes applied on the prostatic neurovascular bundles after nerve‐sparing robot‐assisted radical prostatectomy: a phase II study. BJU Int2018; 121: 473–9
- 5 Rodríguez‐Vázquez M, Vega‐Ruiz B, Ramos‐Zúñiga R, Saldaña‐Koppel DA, Quiñones‐Olvera LF. Chitosan and its potential use as a scaffold for tissue engineering in regenerative medicine. Biomed Res Int2015; 2015: 821279
Video: Chitosan membranes applied on the prostatic neurovascular bundles after nerve‐sparing robot‐assisted radical prostatectomy: a phase II study
Chitosan membranes applied on the prostatic neurovascular bundles after nerve‐sparing robot‐assisted radical prostatectomy: a phase II study
Abstract
Objective
To evaluate the feasibility and the safety of applying chitosan membrane (ChiMe) on the neurovascular bundles (NVBs) after nerve‐sparing robot‐assisted radical prostatectomy (NS‐RARP). The secondary aim of the study was to report preliminary data and in particular potency recovery data.
Patients and Methods
This was a single‐centre, single‐arm prospective study, enrolling all patients with localised prostate cancer scheduled for RARP with five‐item version of the International Index of Erectile Function scores of >17, from July 2015 to September 2016. All patients underwent NS‐RARP with ChiMe applied on the NVBs. The demographics, perioperative, postoperative and complications data were evaluated. Potency recovery data were evaluated in particular and any sign/symptom of local allergy/intolerance to the ChiMe was recorded and evaluated.
Results
In all, 140 patients underwent NS‐RARP with ChiMe applied on the NVBs. Applying the ChiMe was easy in almost all the cases, and did not compromise the safety of the procedure. None of the patients reported signs of intolerance/allergy attributable to the ChiMe and potency recovery data were encouraging.
Conclusion
In our experience, ChiMe applied on the NVBs after NS‐RARP was feasible and safe, without compromising the duration, difficulty or complication rate of the ‘standard’ procedure. No patients had signs of intolerance/allergy attributable to the ChiMe and potency recovery data were encouraging. A comparative cohort would have added value to the study. The present paper was performed before Conformité Européene (CE)‐mark achievement.