Editorial: Too many men still undergo needless prostate biopsy
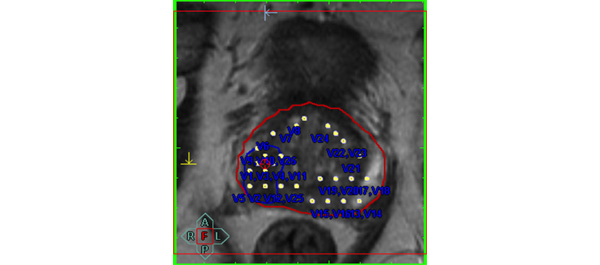
Multiple studies have shown that only one in three or four men with a raised PSA level prove to have prostate cancer and many men suffer potentially life-threatening complications from transrectal prostate biopsy. There is an urgent need for better risk stratification of men with elevated PSA levels. Any such test should have a high negative predicative value (NPV; small number of significant cancers missed) but also a high positive predictive value (PPV; i.e. the yield would be high and there would be very few false positives) to diminish the number of unnecessary biopsies. Multiparametric MRI (mpMRI) of the prostate, especially with a stronger 3 T magnet, has been advocated for this purpose. The parameters refer to the separate MRI sequences used, typically at least three. Sequences can not only study the anatomy of the gland (standard T2-weighted MRI), but there is also a measure of the tissue cellularity (diffusion-weighted MRI), vascularity (dynamic contrast-enhanced MRI) or biochemistry (magnetic resonance spectroscopy). Initial data have shown promise but the changes seen on these various sequences can be subtle and interpretation is subjective. Naturally observer experience plays a large part but a standardised scoring system, the so called Prostate Imaging Reporting and Data System (PIRADS) system, has been proposed to improve reporting performance [1]. Each parameter is scored on a scale of 1–5 according to the likelihood of cancer. Scoring systems are always a compromise between the NPV and PPV, and so far there is no agreement where the threshold for each parameter should be set. In the original document, the authors proposed that a score of 4 or 5 signifies a high likelihood or almost certainty of cancer, whilst scores of 1 or 2 denote a high likelihood of benign tissue. A score of 3 is evens. The paper by Kuru et al. [2] shows a high NPV only when the threshold was set at the low level of 2 for each parameter. Predictably, at this threshold the PPV was extremely low, and therefore many men would still undergo unnecessary biopsy. Another similar paper advocated a mean threshold of 3, but even then the PPV was 38% with a NPV of 95% [3]. Both these papers are retrospective studies, in particular the MRI readings were done retrospectively. Nevertheless, the low PPV is disappointing. The results of prospective studies with multiple readers are keenly awaited and I hope that that these will find a higher PPV for mpMRI, and we can to move to an era when fewer men undergo needless prostate biopsy.
Uday Patel
St George’s Hospital, London, UK
References
- Barentsz JO, Richenberg J, Clements R et al. ESUR prostate MR guidelines 2012. Eur Radiol 2012; 22: 746–757
- Kuru T, Roethke M, Rieker P et al. Histology core-specific evaluation of the European Society of Urogenital Radiology (ESUR) standardised scoring system of multiparametric magnetic resonance imaging (mpMRI) of the prostate. BJU Int 2013; 112:1080–1087
- Portalez D, Mozer P, Cornud F et al. Validation of the European Society of Urogenital Radiology scoring system for prostate cancer diagnosis on multiparametric magnetic resonance imaging in a cohort of repeat biopsy patients. Eur Urol 2012; 62: 986–996