Article of the Month: Bladder cancer: diagnosis and management of bladder cancer
Every month the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation. There is also a podcast created by a Urology Resident.
If you only have time to read one article this week, it should be this one.
Introduction
Bladder cancer is the seventh most common cancer in the UK. It is 3–4 times more common in men than in women. In the UK in 2011, it was the fourth most common cancer in men and the thirteenth most common in women. There were 10,399 people diagnosed with bladder cancer and 5081 deaths from bladder cancer in 2011. The majority of cases occur in people aged over 60. The main risk factor for bladder cancer is increasing age, but smoking and exposure to some industrial chemicals also increase risk.
Bladder cancer is usually identified on the basis of visible blood in the urine or blood found on urine testing, but emergency admission is a common way for bladder cancer to present, and is often associated with a poor prognosis.
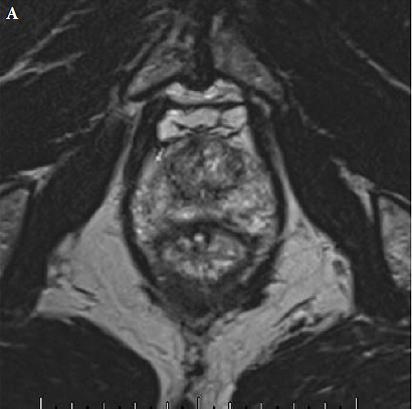
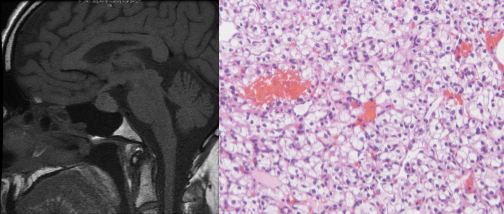
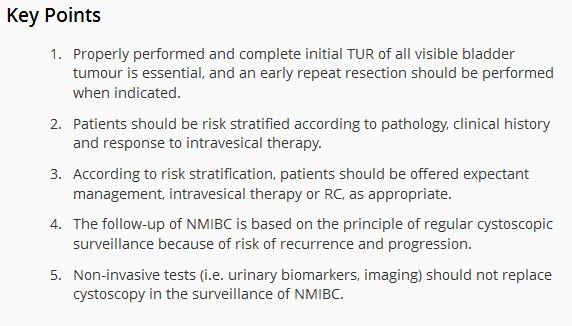
Most bladder cancers (75–80%) do not involve the muscle wall of the bladder and are usually treated by telescopic removal of the cancer (transurethral resection of bladder tumour [TURBT]). This is often followed by instillation of chemotherapy or vaccine-based therapy into the bladder, with prolonged telescopic checking of the bladder (cystoscopy) as follow-up. Some people in this group who are at higher risk are treated with major surgery to remove the bladder (cystectomy). People with cancer in or through the bladder muscle wall may be treated with intent to cure using chemotherapy, cystectomy or radiotherapy, and those who have cancer too advanced to cure may have radiotherapy and chemotherapy.
The involvement of the urogenital tract and the nature of the treatments give this cancer a strong psychological impact, in addition to the physical impact of the disease and its treatments, which is often profound. The prevalence of the condition and the nature of its management make bladder cancer one of the most expensive cancers for the NHS.
There is thought to be considerable variation across the NHS in the diagnosis and management of bladder cancer and the provision of care to people who have it. There is evidence that the patient experience for people with bladder cancer is worse than that for people with other cancers.
This guideline covers adults (18 years and older) referred from primary care with suspected bladder cancer and those with newly diagnosed or recurrent bladder (urothelial carcinoma, adenocarcinoma, squamous-cell carcinoma or small-cell carcinoma) or urethral cancer. There was insufficient high-quality evidence on which to make specific recommendations for non-urothelial bladder cancer (adenocarcinoma, squamous-cell carcinoma or small-cell carcinoma).
It does not cover people aged under 18 or adults with bladder sarcoma, urothelial cancer of the upper urinary tract, or secondary bladder or urethral cancer (for example, bowel or cervix cancer spreading into the bladder).
Medicines
The guideline assumes that prescribers will use a medicine’s summary of product characteristics to inform decisions made with individual patients.
This guideline recommends some medicines for indications for which they do not have a UK marketing authorisation at the date of publication, if there is good evidence to support that use. The prescriber should follow relevant professional guidance, taking full responsibility for the decision. The patient (or those with authority to give consent on their behalf) should provide informed consent, which should be documented. See the General Medical Council’s Prescribing guidance: prescribing unlicensed medicines for further information. Where recommendations have been made for the use of medicines outside their licensed indications (‘off-label use’), these medicines are marked with a footnote in the recommendations.