Urologists in the Yellow Submarine – a Periscope to the World
 Over the last few weeks, there has been a lot of chatter about a new Social Media platform. Just when you thought that we had exhausted all possible ways that people could interact online, live video streaming is the talk of the town.
Over the last few weeks, there has been a lot of chatter about a new Social Media platform. Just when you thought that we had exhausted all possible ways that people could interact online, live video streaming is the talk of the town.
Last month, two competing live video streaming apps were launched. Meerkat initially gained popularity quite rapidly, particularly through Twitter, given the ease and immediacy of being able to share your live video streaming with twitter followers. Twitter acquired its competitor, Periscope, and Meerkat’s access to the twitter followers was cut off no sooner than it had began. Already there are arguments as to which of the two platforms are better but I can already sense from user reactions and expert opinion, that Periscope will be the one that will prevail. The might of Twitter will be very difficult to compete with.
Why on earth would urologists be interested in live broadcasts? The obvious application is live streaming of events such as conferences. The default option is perform a public broadcast and this will have particular value when there is an advocacy focus. There is also an option to broadcast privately only to followers of the Periscope account performing the broadcast. The latter may well be the best option for more sensitive material but there are still issues that need to be sorted out. In particular, there is no simple mechanism to determine which followers should be permitted to follow the broadcasting account in order to see a private live stream. It is inevitable that this will be simplified in the future, as it would be logical for this platform to find a mechanism to attract business users.
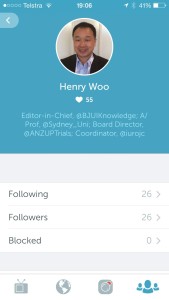
As things are at present, one needs to have a twitter account in order to sign on to broadcast using Periscope. This platform is designed for the mobile user – this is both for broadcasting and for watching the live stream. Attempting to do this on a desktop or laptop website is cumbersome and clumsy from my initial attempts to do so whereas the iOS App was straightforward and intuitive, particularly for those already familiar with the Twitter app.
Note the similarity of the iOS Periscope App with the Twitter App interface.
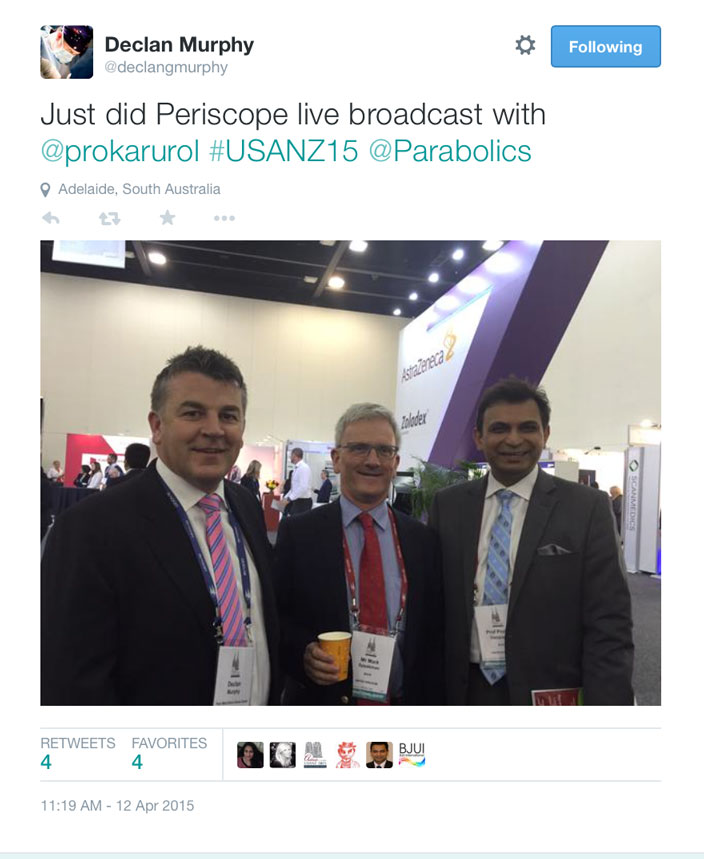
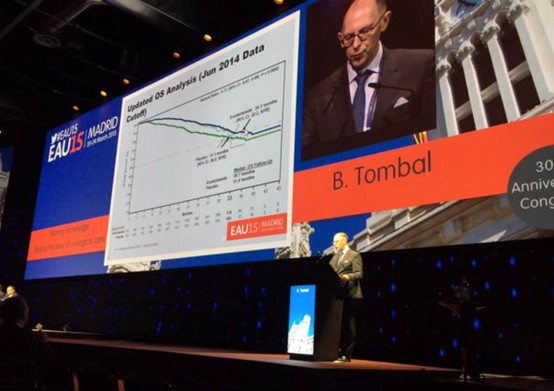
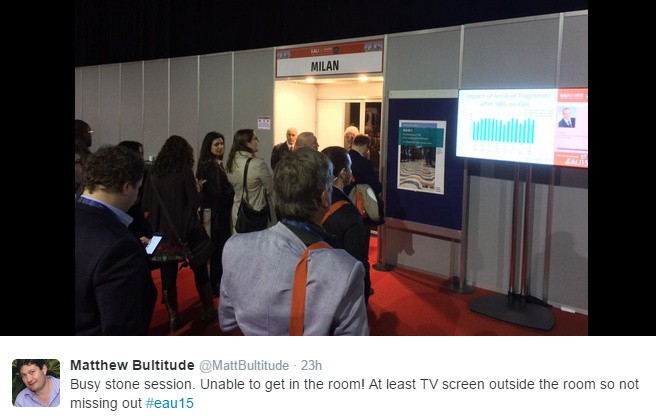
It is my belief that the first ever Periscope live stream broadcast from a medical conference was performed on Sunday 12 April 2015 at the Urological Society of Australia and New Zealand’s (USANZ) Annual Scientific Meeting. Declan Murphy used Periscope to broadcast a message from Prokar Dasgupta, Editor-in-Chief of the BJUI Journal. The video from the Periscope live stream is below. This first, at least for a urological conference, was tweeted by Declan Murphy.
A couple of hours later, I performed a live video stream from the Social Media session when Imogen Patterson gave an excellent presentation on managing our online reputations. During the feed, observers are able to make comments as well as to demonstrate their approval by tapping their screens to trigger a flow of hearts from the bottom right hand corner of the screen.
This is a screenshot from an unrelated live video feed. From the bottom left, the user is notified of those joining the observation of the feed as well as comments. From the bottom right, hearts float upwards in response to positive taps of the screen by watchers.
There are a few issues with Periscope as it is right now. The feed is only available for 24 hours before disappearing from the Periscope platform, however, a video recording minus the comments and hearts, can be stored in the photo stream on your mobile device. As mentioned before, you must have a twitter account to broadcast although you do not need one to view a broadcast. Thirdly, directed broadcasting should be simplified.
Social media platforms come and go but the ability to live stream is an exciting new development. For Periscope, it is my belief that the potential application for a use in medical education seems boundless. Live broadcasting is no longer the exclusive domain of television and cable networks.
Henry Woo (@drhwoo) is Associate Professor of Surgery at the Sydney Adventist Hospital Clinical School of the University of Sydney. He is the Editor-in-Chief of BJUI Knowledge, an innovative on-line CME portal that launches this year.