The Social Media Revolution in Chinese Urology
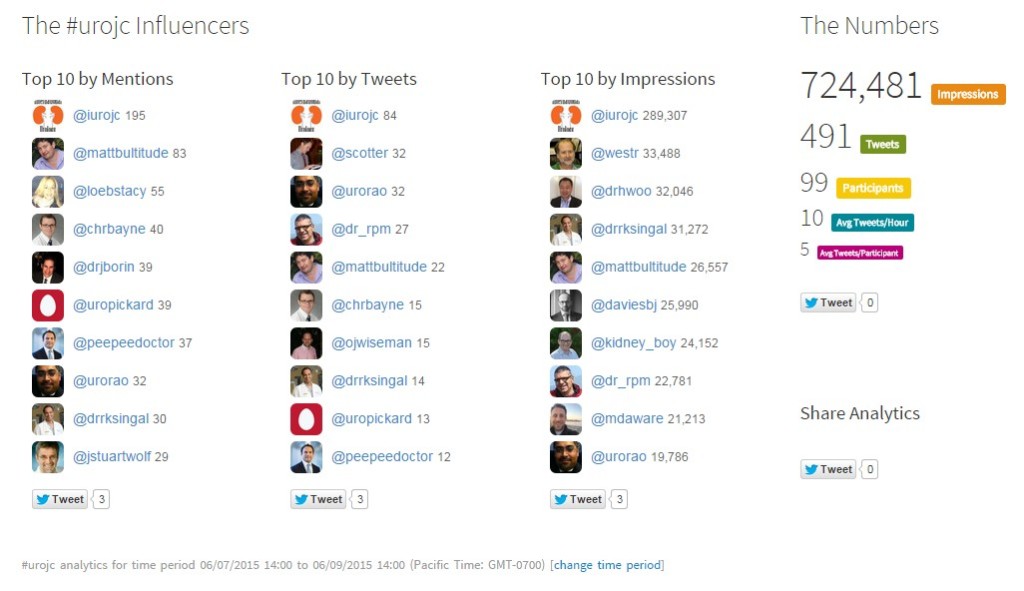
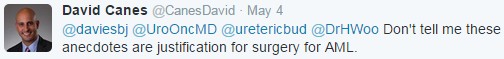
 It is well known that Twitter, Facebook and YouTube, the most popular social media platforms available in the West, are not easily accessible in China. It is also clear that urologists in the West have embraced these social media platforms (Twitter in particular), not just for personal interaction, but also for professional engagement, and journals such as BJUI have enthusiastically encouraged the use of social media for urologists through their use of Twitter, blogging, YouTube etc.
It is well known that Twitter, Facebook and YouTube, the most popular social media platforms available in the West, are not easily accessible in China. It is also clear that urologists in the West have embraced these social media platforms (Twitter in particular), not just for personal interaction, but also for professional engagement, and journals such as BJUI have enthusiastically encouraged the use of social media for urologists through their use of Twitter, blogging, YouTube etc.
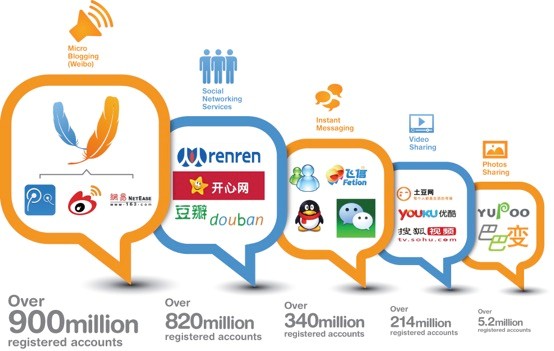
So what then of Chinese urology? Are we missing out on all this? Not at all! In fact, as a recent BMJ blog observed, China is among the most heavily connected populations on earth, and the smartphone revolution has seen this connectivity grow very rapidly in recent years, more than in many Western countries. The lack of access to Western websites has just meant that a host of home-grown websites have cropped up to allow the insatiable appetite for connectivity to be met. Therefore sites such as RenRen (like Facebook), Sina Weibo (like Twitter), and Youku (like YouTube). The BMJ have blogged about this and have highlighted the huge volume of activity on Chinese social media sites.
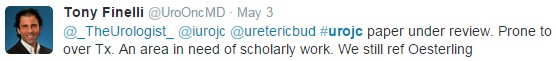
Figure from “Your quick guide to social media strategy in China”
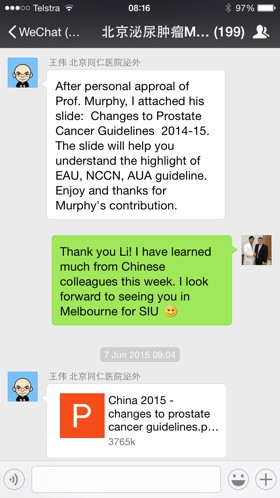
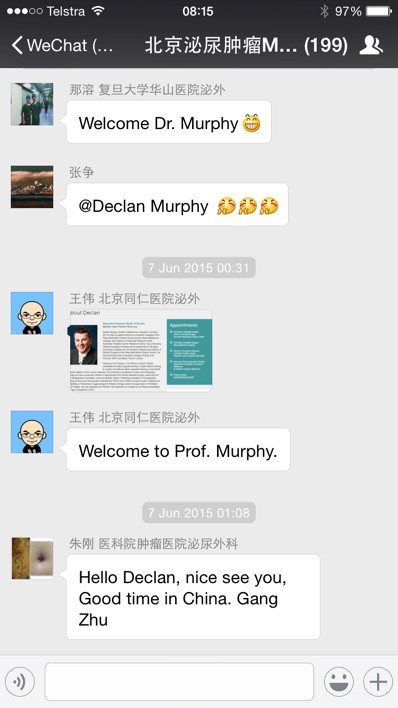
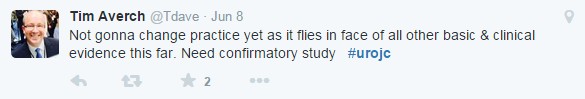
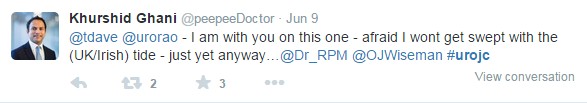
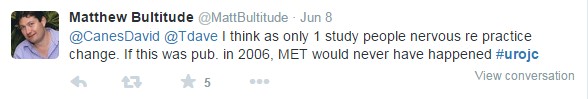
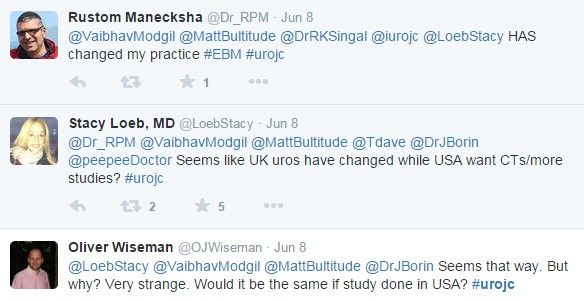
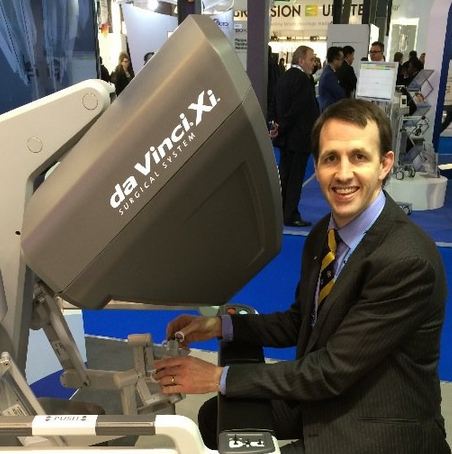
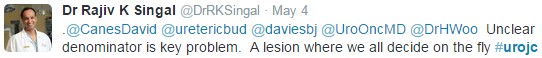
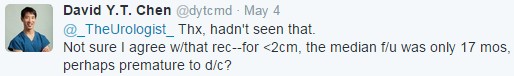
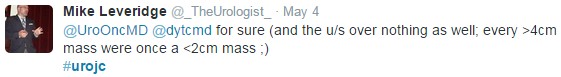
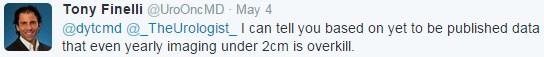
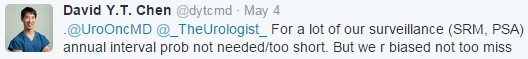
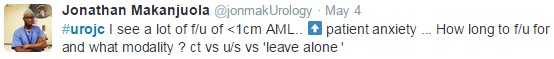
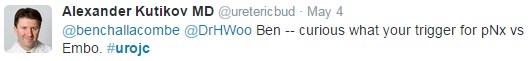
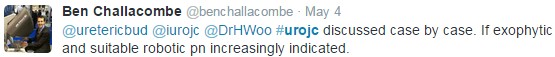
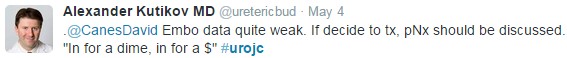
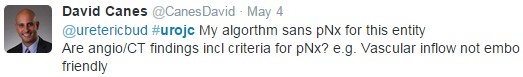
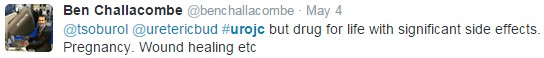
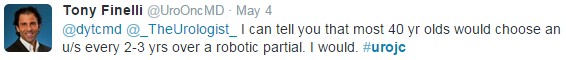
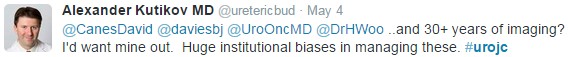
At present, the most popular platform among Chinese urologists is WeChat. WeChat, (similar to WhatsApp), is connecting more than a half billion Chinese people now. Apart from free chat, video and voice call, group chat is perfect for professional online discussion. There are several major urological discussion groups. Each group has many hundreds of participants. It is estimated that more 3000 urologists (1/4) in China have been involved in one or more online discussion group. Earlier this month, Prof. Declan Murphy’s lecture slides were uploaded to our urology major discussion group after his presentation at the Asia Urology Prostate Cancer Forum in Shanghai.
More than 2000 Chinese urologists (1/6) watched his slides on smartphones that weekend and shared feedback using the app. Prof Murphy, one of the world’s foremost leaders in social media, even joined WeChat and engaged in dialogue with the discussion group.
At present, the top two most famous discussion groups are called scope art and Hippocrates group. A talented young urologist, Dr. QIan Zhang, set up scope art two years ago. More than 500 urologists from across the country were invited to join the group. New knowledge, case discussion and meeting information can be arranged in the group. Recently, the Top 10 WeChat urologists has been selected thorough WeChat vote platform system. More than 20,000 WeChat users voted for their favorite social medial stars. Several discussion groups were built based on the different specialties (stone disease, andrology etc.). Several leading uro-oncologists, urologists, pathologists, radiologists and related experts also built an MDT discussion group to discuss interesting uro-oncology cases to help select the best options for patients.
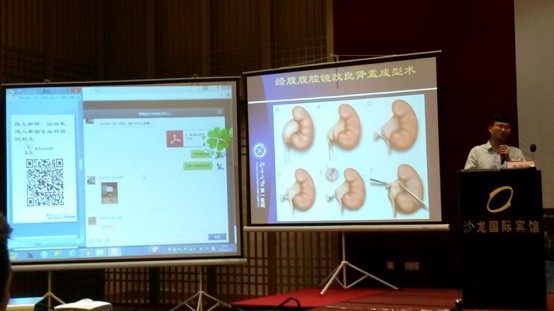
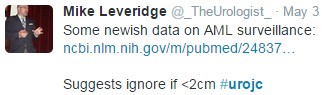
We are now also seeing these online discussions develop a physical presence. Recently, a WeChat integrated Hippocrates urological meeting was held in Jiaxing. When each speaker starts to talk, the slides were uploaded to the WeChat discussion group, allowing the entire membership of the discussion group to attach their comments and questions during the presentation. All the questions and comments are projected to the separate screen in the meeting hall. The speaker can discuss with all the members, wherever they are.
WeChat meeting in action in Jiaxing
As these examples demonstrate, social media significantly helps Chinese urologists communicate more effectively, especially in such a large country with a huge population. We are very keen to embrace these new communication platforms and to engage more with our colleagues in the West!
Dr. Wei Wang
Consultant Urologist, Beijing Tongren Hospital, Capital Medical University, China
WeChat ID: medtrip