Article of the Week: Evaluation of Sig24, a 24-gene signature
Every week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video discussing the paper.
If you only have time to read one article this week, it should be this one.
Evaluation of a 24-gene signature for prognosis of metastatic events and prostate cancer-specific mortality
How to Cite
Pellegrini, K. L., Sanda, M. G., Patil, D., Long, Q., Santiago-Jiménez, M., Takhar, M., Erho, N., Yousefi, K., Davicioni, E., Klein, E. A., Jenkins, R. B., Karnes, R. J. and Moreno, C. S. (2017), Evaluation of a 24-gene signature for prognosis of metastatic events and prostate cancer-specific mortality. BJU International, 119: 961–967. doi: 10.1111/bju.13779
Abstract
Objectives
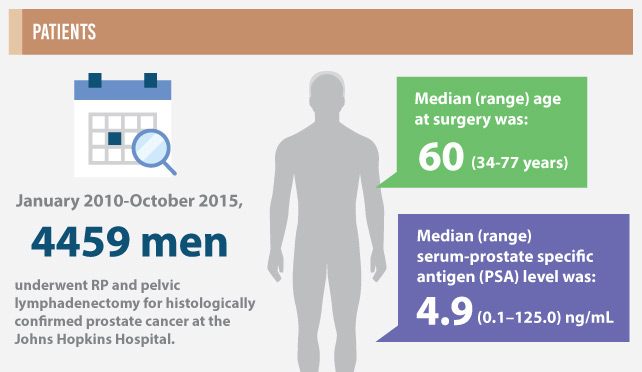
To determine the prognostic potential of a 24-gene signature, Sig24, for identifying patients with prostate cancer who are at risk of developing metastases or of prostate cancer-specific mortality (PCSM) after radical prostatectomy (RP).
Patients and Methods
Sig24 scores were calculated from previously collected gene expression microarray data from the Cleveland Clinic and Mayo Clinic (I and II). The performance of Sig24 was determined using time-dependent c-index analysis, Cox proportional hazards regression and Kaplan–Meier survival analysis.
Results
Higher Sig24 scores were significantly associated with higher pathological Gleason scores in all three cohorts. Analysis of the Mayo Clinic II cohort, which included time-to-event information, indicated that patients with high Sig24 scores also had a higher risk of developing metastasis (hazard ratio [HR] 3.78, 95% confidence interval [CI]: 1.96–7.29; P < 0.001) or of PCSM (HR 6.54, 95% CI: 2.16–19.83; P < 0.001).
Conclusions
The findings of the present study show the applicability of Sig24 for the prognosis of metastasis or PCSM after RP. Future studies investigating the combination of Sig24 with available prognostic tests may provide new approaches to improve risk stratification for patients with prostate cancer.